Quetiapine
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /kwᵻˈtaɪ.əpiːn/ kwi-TY-ə-peen |
| Trade names | Seroquel |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a698019 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | N05AH04 (WHO) |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 100%[1] |
| Protein binding | 83%[2] |
| Metabolism | Hepatic via CYP3A4-catalysed sulfoxidation to its active metabolite norquetiapine (N-desalkylquetiapine)[3] |
| Biological half-life | 7 hours (parent compound); 9–12 hours (active metabolite, norquetiapine)[2][4] |
| Excretion | Renal (73%), faeces (20%)[1][2][4][5] |
| Identifiers | |
| |
| CAS Number |
111974-69-7 |
| PubChem (CID) | 5002 |
| IUPHAR/BPS | 50 |
| DrugBank |
DB01224 |
| ChemSpider |
4827 |
| UNII |
BGL0JSY5SI |
| KEGG |
D08456 |
| ChEBI |
CHEBI:8707 |
| ChEMBL |
CHEMBL716 |
| ECHA InfoCard | 100.131.193 |
| Chemical and physical data | |
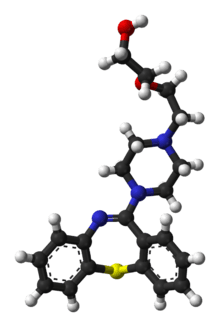
| Formula | C21H25N3O2S |
| Molar mass | 383.5099 g/mol |
| 3D model (Jmol) | Interactive image |
| Solubility in water | 3.29 mg/mL (20 °C) |
| |
| |
| (verify) | |
Quetiapine, marketed as Seroquel, is an atypical antipsychotic approved for the treatment of schizophrenia, bipolar disorder, and along with an antidepressant to treat major depressive disorder. It is also sometimes used as a sleep aid because of its sedating effect but this use is not recommended.[6]
Annual sales are approximately $1.3 billion worldwide.[7] Quetiapine was developed by AstraZeneca from 1992 to 1996. It was first approved by the FDA in 1997. There are now several generic versions.[8]
Medical uses


Quetiapine is primarily used to treat schizophrenia or bipolar disorder.[9]
Schizophrenia
A second Cochrane Review[10] comparing quetiapine to typical antipsychotics concluded that quetiapine
- Has efficacy against positive symptoms that appears no better than typical antipsychotics, but might be more efficacious for negative symptoms.
- Has discontinuation rates similar to those of typical antipsychotics, but fewer of these discontinuations were due to adverse events.
- Produces fewer side effects, particularly movement related side effects.
- Produces suicide attempt, suicide, death, QTc prolongation, low blood pressure, tachycardia, sedation, gynaecomastia, galactorrhoea, menstrual irregularity and white blood cell count at a rate similar to first generation antipsychotics.[11]
There is tentative evidence of the benefit of quetiapine versus placebo in schizophrenia; however, definitive conclusions are not possible due to the high rate of attrition in trials (greater than 50%) and the lack of data on economic outcomes, social functioning, or quality of life.[12]
It is debatable whether, as a class, typical or atypical antipsychotics are more effective.[13] Both have equal drop-out and symptom relapse rates when typicals are used at low to moderate dosages.[14] While quetiapine has lower rates of extrapyramidal side effects, there is greater sleepiness and rates of dry mouth.[12]
A Cochrane Review comparing quetiapine to other atypical antipsychotic agents tentatively concluded that it may be less efficacious than olanzapine and risperidone; produce fewer movement related side effects than paliperidone, aripiprazole, ziprasidone, risperidone and olanzapine; and produce weight gain similar to risperidone, clozapine and aripiprazole.[11]
Bipolar disorder
In those with bipolar disorder, quetiapine is used to treat depressive episodes, acute manic episodes associated with bipolar I disorder (as either monotherapy or adjunct therapy to lithium, valproate or lamotrigine), and maintenance treatment of bipolar I disorder (as adjunct therapy to lithium or divalproex).[15][16]
Major depressive disorder
Quetiapine is effective when used by itself[17] and when used along with other medications in major depressive disorder (MDD).[17][18] However, sedation is often an undesirable side effect.[17]
In the United States,[4] the United Kingdom[19] and Australia (in this indication it isn't covered by the Pharmaceutical Benefits Scheme), quetiapine is licensed for use as an adjunct in the treatment of MDD.[20]
Alzheimer's disease
Quetiapine does not decrease agitation among people with Alzheimer's. Quetiapine worsens intellectual functioning in the elderly with dementia and therefore is not recommended.[21]
Other
The use of low doses of quetiapine for insomnia, while common, is not recommended; there is little evidence of benefit and concerns regarding adverse effects.[22][23]
It is sometimes used off-label, often as an augmentation agent, to treat conditions such as Tourette syndrome,[24] musical hallucinations[25] and anxiety disorders.[26]
Quetiapine and clozapine are the most widely used medications for the treatment of Parkinson's disease psychosis due to their very low extrapyramidal side effect liability. Owing to the risks associated with clozapine (e.g. agranulocytosis, diabetes mellitus, etc.), clinicians often attempt treatment with quetiapine first, although the evidence to support quetiapine's use for this indication is significantly weaker than that of clozapine.[27][28]
Adverse effects
Sources for incidence lists:[1][4][19][20][28][29]
- Very common (>10% incidence) adverse effects
- Dry mouth
- Dizziness
- Headache
- Somnolence (drowsiness; of 15 antipsychotics quetiapine causes the 5th most sedation. Extended release (XR) formulations tend to produce less sedation, dose-by-dose than the immediate release formulations)[30]
- Common (1–10% incidence) adverse effects
- High blood pressure
- Orthostatic hypotension
- High pulse rate
- High blood cholesterol
- Elevated serum triglycerides
- Abdominal pain
- Constipation
- Increased appetite
- Vomiting
- Increased liver enzymes
- Backache
- Asthenia
- Insomnia
- Lethargy
- Tremor
- Agitation
- Nasal congestion
- Pharyngitis
- Fatigue
- Pain
- Dyspepsia (Indigestion)
- Peripheral oedema
- Dysphagia
- Extrapyramidal disease: quetiapine and clozapine are noted for their relative lack of extrapyramidal side effects[19][28][30]
- Weight gain: SMD 0.43 kg when compared to placebo. Produces roughly as much weight gain as risperidone, less weight gain than clozapine, olanzapine and zotepine and more weight gain than ziprasidone, lurasidone, aripiprazole and asenapine.[30] As with many other atypical antipsychotics this action is likely due to its actions at the H1 histamine receptor and 5-HT2C receptor.[3]
- Rare (<1% incidence) adverse effects
- Prolonged QT interval (had an odds ratio for prolonging the QT interval over placebo of 0.17)[30]
- Sudden cardiac death
- Syncope
- Diabetic ketoacidosis
- Restless legs syndrome
- Hyponatraemia, low blood sodium.
- Jaundice, yellowing of the eyes, skin and mucous membranes due to an impaired ability of the body to clear bilirubin, a by product of haem breakdown.
- Pancreatitis, pancreas swelling.
- Agranulocytosis, a potentially fatal drop in white blood cell count.
- Leukopenia, a drop in white blood cell count, not as severe as agranulocytosis.
- Neutropenia, a drop in neutrophils, the cell of the immune cells that defends the body against bacterial infections.
- Eosinophilia
- Anaphylaxis, a potentially fatal allergic reaction.
- Seizure
- Hypothyroidism, underactive thyroid gland.
- Myocarditis, swelling of the myocardium.
- Cardiomyopathy
- Hepatitis, swelling of the liver.
- Suicidal ideation
- Priapism. A prolonged and painful erection.
- Stevens-Johnson syndrome. A potentially fatal skin reaction.
- Neuroleptic malignant syndrome a rare and potentially fatal complication of antipsychotic drug treatment. It is characterised by the following symptoms: tremor, rigidity, hyperthermia, tachycardia, mental status changes (e.g. confusion), etc.
- Tardive Dyskinesia. A rare and often irreversible neurological condition characterised by involuntary movements of the face, tongue, lips and rest of the body. Most commonly occurs after prolonged treatment with antipsychotics. It is believed to be particularly uncommon with atypical antipsychotics, especially quetiapine and clozapine[20][31]
Both typical and atypical antipsychotics can cause tardive dyskinesia.[32] According to one study, rates are lower with the atypicals at 3.9% as opposed to the typicals at 5.5%.[32] Although Quetiapine and Clozapine are atypical antipsychotics, switching to these atypicals is an option to minimize symptoms of tardive dyskinesia caused by other atypicals.[33]
Weight gain can be a problem for some, with quetiapine causing more weight gain than fluphenazine, haloperidol, loxapine, molindone, olanzapine, pimozide, risperidone, thioridazine, thiothixene, trifluoperazine, and ziprasidone, but less than chlorpromazine, clozapine, perphenazine, and sertindole.[34]
Studies conducted on beagles have resulted in the formation of cataracts. While there are reports of cataracts occurring in humans, controlled studies including thousands of patients have not demonstrated a clear causal association between quetiapine therapy and this side-effect. However, the Seroquel website[35] still recommends users have eye examinations every six months.
As with some other anti-psychotics, quetiapine may lower the seizure threshold,[36] and should be taken with caution in combination with drugs such as bupropion.
Discontinuation
Quetiapine should be discontinued gradually, with careful consideration from the prescribing doctor, to avoid withdrawal symptoms or relapse.
The British National Formulary recommends a gradual withdrawal when discontinuing anti-psychotic treatment to avoid acute withdrawal syndrome or rapid relapse.[37] Due to compensatory changes at dopamine, serotonin, adrenergic and histamine receptor sites in the central nervous system, withdrawal symptoms can occur during abrupt or over-rapid reduction in dosage. However, despite increasing demand for safe and effective antipsychotic withdrawal protocols or dose-reduction schedules, no specific guidelines with proven safety and efficacy are currently available.
Withdrawal symptoms reported to occur after discontinuation of antipsychotics include nausea, emesis, lightheadedness, diaphoresis, dyskinesia, orthostatic hypotension, tachycardia, insomnia, nervousness, dizziness, headache, excessive non-stop crying, and anxiety.[38][39] Some have argued that additional somatic and psychiatric symptoms associated with dopaminergic super-sensitivity, including dyskinesia and acute psychosis, are common features of withdrawal in individuals treated with neuroleptics.[40][41]
Overdosage
Most instances of acute overdosage result only in sedation, hypotension and tachycardia, but cardiac arrhythmia, coma and death have occurred in adults. Serum or plasma quetiapine concentrations are usually in the 1–10 mg/L range in overdose survivors, while postmortem blood levels of 10–25 mg/L are generally observed in fatal cases.[42] Non-toxic levels in postmortem blood extend to around 0.8 mg/kg, but toxic levels in postmortem blood can begin at 0.35 mg/kg.[43][44]
Pregnancy and lactation
Placental exposure is least for quetiapine compared to other atypical antipsychotics.[28] The evidence is insufficient to rule out any risk to the foetus but available data suggests it is unlikely to result in any major foetal malformations.[2][5][29] It is secreted in breast milk and hence quetiapine-treated mothers are advised not to breastfeed.[2][5][29]
Pharmacology
| Receptor | Quetiapine (Cloned human receptors) |
Norquetiapine (Cloned human receptors) |
|---|---|---|
| D1 | 994.5 | 99.8 (Rat receptor) |
| D2 | 379 | 196 |
| D3 | 340 | - |
| D4 | 2019 | - |
| 5-HT1A | 394.2 | 45 |
| 5-HT2A | 118 | 48 |
| 5-HT2C | 1843 | 107 |
| 5-HT6 | 33 / 1864 | - |
| 5-HT7 | 307 | 76 |
| α1A | 22 | 144 |
| α1B | 14.6 | 46.4 (Rat receptor) |
| α2A | 3630 | 237 |
| α2C | 28.85 | - |
| H1 | 6.9 | 3.5 |
| H2 | 41.24 | - |
| M1 | 489 | 38.3 (Rat receptor) |
| M3 | 1631.5 | - |
| NET | >10000 | 12 |
Quetiapine has the following pharmacological actions:[49][50][51][52]
- D1 (IC50 = 1268nM), D2 (IC50 = 329nM), D3, and D4 receptor antagonist
- 5-HT1A (IC50 = 717nM) partial agonist, 5-HT2A (IC50 = 148nM), 5-HT2C, and 5-HT7 receptor antagonist
- α1-adrenergic (IC50 = 94nM) and α2-adrenergic receptor (IC50 = 271nM) antagonist
- H1 receptor (IC50 = 30nM) antagonist
- mACh receptor (IC50 = >5000nM) antagonist
This means quetiapine is a dopamine, serotonin, and adrenergic antagonist, and a potent antihistamine with clinically negligible anticholinergic properties. Quetiapine binds strongly to serotonin receptors; the drug acts as partial agonist at 5-HT1A receptors.[53] Serial PET scans evaluating the D2 receptor occupancy of quetiapine have demonstrated that quetiapine very rapidly disassociates from the D2 receptor.[54] Theoretically, this allows for normal physiological surges of dopamine to elicit normal effects in areas such as the nigrostriatal and tuberoinfundibular pathways, thus minimizing the risk of side-effects such as pseudo-parkinsonism as well as elevations in prolactin.[55] Some of the antagonized receptors (serotonin, norepinephrine) are actually autoreceptors whose blockade tends to increase the release of neurotransmitters.

Synthesis
The synthesis of quetiapine begins with a dibenzothiazepinone. The lactam is first treated with phosphoryl chloride to produce a dibenzothiazepine. A nucleophilic substitution is used to introduce the sidechain.[56]

Dosage
At very low doses, quetiapine acts primarily as a histamine receptor blocker (antihistamine) and α1-adrenergic blocker. When the dose is increased, quetiapine activates the adrenergic system and binds strongly to serotonin receptors and autoreceptors. At high doses, quetiapine starts blocking significant amounts of dopamine receptors.[57][58] Off-label prescriptions, e.g. for chronic insomnia, of low-dose quetiapine is not recommended due to the harmful side-effects.[59]
Due to compensatory changes at dopamine, serotonin, adrenergic and histamine receptor sites in the central nervous system, a gradual reduction in dosage is recommended to minimise or avoid withdrawal symptoms. Withdrawal symptoms reported to occur after discontinuation of quetiapine include trouble sleeping, nausea, vomiting, lightheadedness, sweating, feeling light headed when standing, fast heart rate, as well as nervousness, dizziness, headache, and anxiety. The present evidence suggests that these symptoms affect a small number of susceptible individuals treated with quetiapine.[38]
The British National Formulary recommends a gradual withdrawal when discontinuing antipsychotic treatment to avoid acute withdrawal syndrome or rapid relapse.[37]
Sustained-release
AstraZeneca submitted a new drug application for a sustained-release version of quetiapine in the United States, Canada, and the European Union in the second half of 2006 for treatment of schizophrenia.[60][61] AstraZeneca will retain the exclusive right to market sustained-release quetiapine until 2017. The sustained-release quetiapine is marketed mainly as Seroquel XR. Other marketing names are Seroquel Prolong, Seroquel Depot and Seroquel XL
On May 18, 2007, AstraZeneca announced that the U.S. FDA approved Seroquel XR for acute treatment of schizophrenia.[62] During its 2007 Q2 earnings conference, AstraZeneca announced plans to launch Seroquel XR in the U.S. during August 2007.[63] However, Seroquel XR has become available in U.S. pharmacies only after the FDA approved Seroquel XR for use as maintenance treatment for schizophrenia, in addition to acute treatment of the illness, on November 16, 2007.[64] The company has not provided a reason for the delay of Seroquel XR's launch.
Health Canada approved sale of Seroquel XR on September 27, 2007.[65]
The FDA approved Seroquel XR for the treatment of bipolar depression and bipolar mania in early October 2008. According to AstraZeneca, Seroquel XR is "the first medication approved by the FDA for the once-daily acute treatment of both depressive and manic episodes associated with bipolar."
On July 31, 2008, Handa Pharmaceuticals, based in Fremont, California, announced that its abbreviated new drug application (“ANDA”) for quetiapine fumarate extended-release tablets, the generic version of AstraZeneca’s SEROQUEL XR, has been accepted by the FDA.
On December 1, 2008, Biovail announced that the FDA had accepted the company's ANDA to market its own version of sustained-release quetiapine.[66] Biovail's sustained-release tablets will compete with AstraZeneca's Seroquel XR.
On December 24, 2008, AstraZeneca notified shareholders that the FDA had asked for additional information on the company's application to expand the use of sustained-release quetiapine for treatment of depression.[67]
Society and culture
Regulatory status
In the United States, the Food and Drug Administration (FDA) has approved quetiapine for the treatment of schizophrenia and of acute manic episodes associated with bipolar disorder (bipolar mania) and for treatment of bipolar depression.[68] In 2009, quetiapine XR was approved as adjunctive treatment of major depressive disorder.[69]
Quetiapine received its initial indication from U.S. FDA for treatment of schizophrenia in 1997.[70] In 2004, it received its second indication for the treatment of mania-associated bipolar disorder.[71] In 2007 and 2008, studies were conducted on quetiapine’s efficacy in treating generalized anxiety disorder and major depression.
Cost
In the United States as of 2015 the branded extended release 400 mg pills cost between 9.68 and 23.16 USD each.[72]
Lawsuits
In April 2010, AstraZeneca settled a longstanding U. S. Department of Justice investigation into its aggressive marketing of Seroquel for such off-label uses with a $520-million fine.[68] According to the Department of Justice, "the company recruited doctors to serve as authors of articles that were ghostwritten by medical literature companies and about studies the doctors in question did not conduct. AstraZeneca then used those studies and articles as the basis for promotional messages about unapproved uses of Seroquel."[68]
Multiple lawsuits have been filed in relation to quetiapine's side-effects, in particular, diabetes.[73][74][75][76]
Approximately 10,000[77] lawsuits[78] have been filed against AstraZeneca alleging that quetiapine caused problems ranging from slurred speech and chronic insomnia to deaths.
Controversy
In 2004, a young man named Dan Markingson committed suicide in a controversial Seroquel clinical trial at the University of Minnesota while under an involuntary commitment order.[79] A group of University of Minnesota bioethicists charged that the trial involved an alarming number of ethical violations.[80]
Nurofen Plus tampering case
In August 2011, the UK's Medicines and Healthcare products Regulatory Agency (MHRA) issued a class-4 drug alert following reports that some batches of Nurofen plus contained Seroquel XL instead.[81]
Following the issue of the Class-4 Drug Alert, Reckitt Benckiser (UK) Ltd received further reports of rogue blister strips in cartons of two additional batches of Nurofen Plus tablets. One of the new batches contained Seroquel XL 50 mg tablets and one contained the Pfizer product Neurontin 100 mg capsules.
Following discussions with the MHRA's Defective Medicines Report Centre (DMRC), Reckitt Benckiser (UK) Ltd decided to recall all remaining unexpired stock of Nurofen Plus tablets in any pack size, leading to a Class-1 Drug Alert.[82] The contamination was later traced to in-store tampering by a customer.[83]
References
- 1 2 3 "quetiapine (Rx) - Seroquel, Seroquel XR". Medscape Reference. WebMD. Retrieved 11 October 2013.
- 1 2 3 4 5 "Quetiapine 25 mg film-coated tablets - Summary of Product Characteristics". electronic Medicines Compendium. Sandoz. January 2013. Retrieved 20 October 2013.
- 1 2 Brunton, L; Chabner, B; Knollman, B (2010). Goodman and Gilman’s The Pharmacological Basis of Therapeutics (12th ed.). McGraw Hill Professional. ISBN 978-0071624428.
- 1 2 3 4 Truven Health Analytics, Inc. DrugPoint® System (Internet) [cited 2013 Sep 18]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- 1 2 3 "QUETIAPINE FUMARATE tablet QUETIAPINE FUMARATE (quetiapine fumarate ) tablet [Ascend Laboratories, LLC]". DailyMed. Ascend Laboratories, LLC. October 2013. Retrieved 26 November 2013.
- ↑ James J. Gugger; Manouchkathe Cassagnol (2008). "Low-dose quetiapine is not a benign sedative-hypnotic agent.". The American Journal on Addictions. 17 (5): 454–455. doi:10.1080/10550490802266185. PMID 18770092.
- ↑ "www.sec.gov".
- ↑ "Quepin Full Prescribing Information in Drug Reference Encyclopedia". Retrieved 2010-04-03.
- ↑ "quetiapine-fumarate". The American Society of Health-System Pharmacists. Retrieved 3 April 2011.
- ↑ Suttajit S, Srisurapanont M, Xia J, Suttajit S, Maneeton B, Maneeton N (2013). "Quetiapine versus typical antipsychotic medications for schizophrenia". Cochrane Database Syst Rev. 5: CD007815. doi:10.1002/14651858.CD007815.pub2. PMID 23728667.
- 1 2 Asmal L, Flegar SJ, Wang J, Rummel-Kluge C, Komossa K, Leucht S (2013). "Quetiapine versus other atypical antipsychotics for schizophrenia". Cochrane Database Syst Rev. 11: CD006625. doi:10.1002/14651858.CD006625.pub3. PMID 24249315.
- 1 2 Srisurapanont, M; Maneeton, B; Maneeton, N (2004). Srisurapanont, Manit, ed. "Quetiapine for schizophrenia". Cochrane database of systematic reviews (Online) (2): CD000967. doi:10.1002/14651858.CD000967.pub2. PMID 15106155.
- ↑ Kane JM, Correll CU. Pharmacologic treatment of schizophrenia. Dialogues Clin Neurosci. 2010;12(3):345–57. PMID 20954430.
- ↑ Schultz SH, North SW, Shields CG. Schizophrenia: a review. Am Fam Physician. 2007;75(12):1821–9. PMID 17619525.
- ↑ Thase ME, Macfadden W, Weisler RH, Chang W, Paulsson B, Khan A, Calabrese JR (2006). "Efficacy of Quetiapine Monotherapy in Bipolar I and II Depression". Journal of Clinical Psychopharmacology. 26 (6): 600–9. doi:10.1097/01.jcp.0000248603.76231.b7. PMID 17110817.
- ↑ British National Formulary (BNF) 65. Pharmaceutical Pr; 2013. ISBN 978-0857110848
- 1 2 3 Komossa K, Depping AM, Gaudchau A, Kissling W, Leucht S (Dec 8, 2010). "Second-generation antipsychotics for major depressive disorder and dysthymia.". The Cochrane database of systematic reviews (12): CD008121. doi:10.1002/14651858.CD008121.pub2. PMID 21154393.
- ↑ Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC (2013). "Adjunctive Atypical Antipsychotic Treatment for Major Depressive Disorder: A Meta-Analysis of Depression, Quality of Life, and Safety Outcomes". PLoS Med. 10 (3): e1001403. doi:10.1371/journal.pmed.1001403. PMC 3595214
 . PMID 23554581.
. PMID 23554581. - 1 2 3 British National Formulary (BNF) 65. London, UK: Pharmaceutical Press. 2013. p. 235. ISBN 9780857110848.
- 1 2 3 Rossi, S, ed. (2013). Australian Medicines Handbook (2013 ed.). Adelaide: The Australian Medicines Handbook Unit Trust. ISBN 978-0-9805790-9-3.
- ↑ Ballard C, Margallo-Lana M, Juszczak E, Douglas S, Swann A, Thomas A, O'Brien J, Everratt A, Sadler S, Maddison C, Lee L, Bannister C, Elvish R, Jacoby R (2005). "Quetiapine and rivastigmine and cognitive decline in Alzheimer's disease: randomised double blind placebo controlled trial". BMJ. 330 (7496): 874. doi:10.1136/bmj.38369.459988.8F. PMC 556156
 . PMID 15722369.
. PMID 15722369. - ↑ Coe HV, Hong IS (May 2012). "Safety of low doses of quetiapine when used for insomnia". The Annals of pharmacotherapy. 46 (5): 718–22. doi:10.1345/aph.1Q697. PMID 22510671.
- ↑ Maglione M, Maher AR, Hu J, et al. (September 2011). "Off-Label Use of Atypical Antipsychotics: An Update". PMID 22132426.
- ↑ Mukaddes NM, Abali O (2003). "Quetiapine Treatment of Children and Adolescents with Tourette's Disorder". Journal of Child and Adolescent Psychopharmacology. 13 (3): 295–9. doi:10.1089/104454603322572624. PMID 14642017.
- ↑ Oliver Sacks "Musicophilia" Knopf NY 2007 P.67
- ↑ Becker PM (2006). "Treatment of sleep dysfunction and psychiatric disorders". Current Treatment Options in Neurology. 8 (5): 367–375. doi:10.1007/s11940-006-0026-6. PMID 16901376.
- ↑ Shotbolt P, Samuel M, David A (November 2010). "Quetiapine in the treatment of psychosis in Parkinson's disease". Therapeutic Advances in Neurological Disorders. 3 (6): 339–350. doi:10.1177/1756285610389656. PMC 3002640
 . PMID 21179595.
. PMID 21179595. - 1 2 3 4 Taylor, D; Carol, P; Shitij, K (2012). The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. ISBN 9780470979693.
- 1 2 3 "PRODUCT INFORMATION STADA(TM) Quetiapine (quetiapine fumarate Tablets 25 mg, 100 mg, 200 mg, 300 mg)". TGA eBusiness Services. STADA Pharmaceuticals Australia Pty Limited. 30 November 2012. Retrieved 19 September 2013.
- 1 2 3 4 Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lässig B, Salanti G, Davis JM (September 2013). "Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis". The Lancet. 382 (9896): 951–962. doi:10.1016/S0140-6736(13)60733-3. PMID 23810019.
- ↑ Erkan, A; Pirildar, S; Acarer, A; Akdeniz, F (2011). "Efficacy of Low-dose Pramipexole Augmentation in the Treatment of Refractory Psychotic Depression Complicated with Tardive Dyskinesia A Case Report" (PDF). Bulletin of Clinical Psychopharmacology (in Turkish). 21 (4): 353–355. doi:10.5455/bcp.20111029071711.
- 1 2 Correll CU, Schenk EM (March 2008). "Tardive dyskinesia and new antipsychotics". Current opinion in psychiatry. 21 (2): 151–6. doi:10.1097/YCO.0b013e3282f53132. PMID 18332662.
- ↑ Aia PG, Revuelta GJ, Cloud LJ, Factor SA (2011). "Tardive Dyskinesia". Current Treatment Options in Neurology. 13 (3): 231–241. doi:10.1007/s11940-011-0117-x. PMID 21365202.
- ↑ Antipsychotic-Induced Weight Gain: A Comprehensive Research Synthesis Am J Psychiatry 1999;156:1686-1696.
- ↑ Seroquel website
- ↑ Seroquel Prescribing Information
- 1 2 Group, BMJ, ed. (March 2009). "4.2.1". British National Formulary (57 ed.). United Kingdom: Royal Pharmaceutical Society of Great Britain. p. 192.
Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.
- 1 2 Kim DR, Staab JP (May 2005). "Quetiapine discontinuation syndrome". Am J Psychiatry. 162 (5): 1020. doi:10.1176/appi.ajp.162.5.1020. PMID 15863814.
- ↑ Michaelides C, Thakore-James M, Durso R (Jun 2005). "Reversible withdrawal dyskinesia associated with quetiapine". Mov Disord. 20 (6): 769–70. doi:10.1002/mds.20427. PMID 15747370.
- ↑ Miller, R.; Chouinard, G. (Nov 1993). "Loss of striatal cholinergic neurons as a basis for tardive and L-dopa-induced dyskinesias, neuroleptic-induced supersensitivity psychosis and refractory schizophrenia". Biol Psychiatry. 34 (10): 713–38. doi:10.1016/0006-3223(93)90044-E. PMID 7904833.
- ↑ Moncrieff J (Jul 2006). "Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse". Acta Psychiatr Scand. 114 (1): 3–13. doi:10.1111/j.1600-0447.2006.00787.x. PMID 16774655.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 1355–1357.
- ↑ Skov L, Johansen SS, Linnet K (Jan 2015). "Postmortem Femoral Blood Reference Concentrations of Aripiprazole, Chlorprothixene, and Quetiapine". Journal of Analytical Toxicology. 39 (1): 41–44. doi:10.1093/jat/bku121. PMID 25342720.
- ↑ Skov L, Johansen SS, Linnet K (Jul 2015). "Postmortem Quetiapine Reference concentrations in Brain and Blood". Journal of Analytical Toxicology. 39 (7): 557–561. doi:10.1093/jat/bkv072. PMID 26159868.
- ↑ AstraZeneca Pharmaceuticals LP (March 2011). "SEROQUEL (quetiapine fumarate) tablet, extended release". DailyMed. National Library of Medicine. Section 12.2: Pharmacodynamics. Retrieved 2011-04-26.
- ↑ National Institute of Mental Health. PDSD Ki Database (Internet) [cited 2013 Sep 18]. Chapel Hill (NC): University of North Carolina. 1998-2013. Available from: "Archived copy". Archived from the original on November 8, 2013. Retrieved July 5, 2013.
- ↑ Jensen NH, Rodriguiz RM, Caron MG, Wetsel WC, Rothman RB, Roth BL. N-Desalkylquetiapine, a Potent Norepinephrine Reuptake Inhibitor and Partial 5-HT1A Agonist, as a Putative Mediator of Quetiapine’s Antidepressant Activity. Neuropsychopharmacology [Internet]. 2007 Dec 5 [cited 2013 Sep 18];33(10):2303–12. Available from: http://www.nature.com/npp/journal/v33/n10/full/1301646a.html
- ↑ López-Muñoz F, Álamo C. Active metabolites as antidepressant drugs: the role of norquetiapine in the mechanism of action of quetiapine in the treatment of mood disorders. Front Psychiatry [Internet]. 2013 [cited 2013 Sep 19];4:102. Available from: http://www.frontiersin.org/Neuropharmacology/10.3389/fpsyt.2013.00102/abstract
- ↑ AstraZeneca. "Seroquel (quietapine fumarate) tablets" (PDF). 276521.
- ↑ Richelson E, Souder T (November 2000). "Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds". Life Sciences. 68 (1): 29–39. doi:10.1016/S0024-3205(00)00911-5. PMID 11132243.
- ↑ Davis, Kenneth L; Neuropsychopharmacology, American College of (2002). Neuropsychopharmacology: the fifth ... - Google Books. ISBN 978-0-7817-2837-9.
- ↑ "Seroquel Official FDA information, side effects and uses". Drugs.com. Retrieved 2012-07-09.
- ↑ Guzman, F. "Mechanism of action of quetiapine". Psychopharmacology Institute. Retrieved 20 January 2013.
- ↑ Kapur S, Seeman P; Seeman, P (2001). "Does fast dissociation from the dopamine d(2) receptor explain the action of atypical antipsychotics?:a new hypothesis". American Journal of Psychiatry. 158 (3): 360–369. doi:10.1176/appi.ajp.158.3.360. PMID 11229973.
- ↑ Seeman P (2002). "Atypical antipsychotics: mechanism of action". Can J Psychiatry. 47 (1): 27–38. PMID 11873706.
- ↑ Warawa, E. J.; Migler, B. M.; 1988, U.S. Patent 4,879,288.
- ↑ Richelson E, Souder T (November 2000). "Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds". Life Sciences. 68 (1): 29–39. doi:10.1016/S0024-3205(00)00911-5. PMID 11132243.
- ↑ Gefvert O, Lundberg T, Wieselgren IM, Bergström M, Långström B, Wiesel F, Lindström L (April 2001). "D2 and 5HT2A receptor occupancy of different doses of quetiapine in schizophrenia: a PET study". European Neuropsychopharmacology. 11 (2): 105–110. doi:10.1016/S0924-977X(00)00133-4. PMID 11313155.
- ↑ "Drug Use Evaluation: Low Dose Quetiapine (Seroquel/Seroquel XR)" (PDF). Government Executive Media Group. Oregon State. Retrieved 20 January 2016.
- ↑ "AstraZeneca Submits an NDA For Sustained Release Formulation Seroquel XR. For the treatment of schizophrenia." (Press release). AstraZeneca. 2006-07-18. Retrieved 2007-01-01.
- ↑ "AstraZeneca Submits EU and Canadian Regulatory Filings for Sustained Release Formulation SEROQUEL XR for the Treatment of Schizophrenia" (Press release). AstraZeneca. 2006-10-19. Retrieved 2007-01-01.
- ↑ "FDA Approves AstraZeneca's Once-Daily SEROQUEL XR Extended-Release Tablets For The Treatment Of Schizophrenia" (Press release). AstraZeneca. 2007-05-18. Retrieved 2007-08-02.
- ↑ "Second Quarter and Half Year Results 2007" (Press release). AstraZeneca. 2007-07-26. Retrieved 2007-08-02.
- ↑ "Seroquel XR Receives Approval from FDA for Maintenance Treatment of Schizophrenia" (Press release). AstraZeneca. 2007-11-16. Retrieved 2007-12-03.
- ↑ Notice of Compliance Information - Seroquel XR September 27, 2007, retrieved December 3, 2007
- ↑ "Biovail Announces Filing of ANDA for Quetiapine XR Tablets" (Press release). Biovail. 2008-12-01.
- ↑ "AstraZeneca Receives FDA Complete Response Letter on Seroquel XR for Major Depressive Disorder" (Press release). AstraZeneca. 2008-12-24. Retrieved 2008-12-28.
- 1 2 3 "Pharmaceutical Giant AstraZeneca to Pay $520 Million for Off-label Drug Marketing". Justice news, US Department of Justice. Retrieved 2012-07-16.
- ↑ Guzman, F. "Quetiapine Indications: FDA-Approved and Off-label Uses". Psychopharmacology Institute. Retrieved 19 January 2013.
- ↑ "QUETIAPINE FUMARATE". Electronic Orange Book. Food and Drug Administration. April 2007. Retrieved 2007-05-24.
- ↑ "AstraZeneca Receives FDA Approval for SEROQUEL in Bipolar Mania" (Press release). AstraZeneca. 2004-01-13.
- ↑ Langreth, Robert (June 29, 2016). "Decoding Big Pharma's Secret Drug Pricing Practices". Bloomberg. Retrieved 15 July 2016.
- ↑ Ann Knef (2007-08-02). "Seroquel suit claims 'so much' is poured into marketing and away from research". The Madison / St. Clair Record.
- ↑ Phil Milford (2009-03-11). "AstraZeneca May Link Seroquel, Diabetes, Doctor Says". Bloomberg.com. Bloomberg L.P.
- ↑ "AstraZeneca wins bellwether Seroquel case". FiercePharma. 2010-03-19. Retrieved 2012-07-09.
- ↑ "AstraZeneca pays out million dollar damages". The Local. 2010-08-09.
- ↑ "Questions loom over drug for sleepless vets - Marine Corps News | News from Afghanistan & Iraq". Marine Corps Times. Retrieved 2012-07-09.
- ↑ DUFF WILSON Published: July 18, 2011 (2011-07-19). "Heart Warning Added to Label on Popular Antipsychotic Drug". NyTimes. Retrieved 2012-07-09.
- ↑ Elliott, Carl (September–October 2010). "The Deadly Corruption of Clinical Trials". Mother Jones. Retrieved 2 December 2012.
- ↑ Couzin-Frankel, Jennifer (December 7, 2010). "Minnesota bioethicists critique their university". Science. Retrieved 2 December 2012.
- ↑ "Press releases". MHRA. Retrieved 2012-07-09.
- ↑ "Drug Alerts". MHRA. Retrieved 2012-07-09.
- ↑ "BBC News - Nurofen Plus tampering: Christopher McGuire jailed". Bbc.co.uk. 2012-05-28. Retrieved 2012-07-09.
External links
- "Quetiapine". MedlinePlus. The American Society of Health-System Pharmacists, Inc. 2008-09-01.
- NAMI summary
- Internet Drug List summary
- Compound #1802: Quetiapine ChemBank
- U.S. National Library of Medicine: Drug Information Portal - Quetiapine
- Seroquel Adverse Events Reported to the FDA
- Australian Public Assessment Report for Quetiapine (as fumarate)