Direct Xa inhibitor
Direct factor Xa inhibitors ('xabans') are a class of anticoagulant drugs which act directly upon Factor X in the coagulation cascade, without using antithrombin as a mediator.[1]
Clinical uses
Direct factor Xa inhibitors are being used clinically. Clinical trials have shown promise for these compounds as substitutes for the currently administered vitamin K antagonists or low molecular weight heparin. Those trials demonstrated efficacy and safety against warfarin for stroke prevention in atrial fibrillation and against low-molecular-weight heparin for treatment and secondary prevention of venous thromboembolism or for initial treatment and prevention of venous thromboembolism in patients undergoing hip or knee replacement.[2]
Advantages of orally administered direct Xa inhibitors lie in the fact that they have a rapid onset and offset of action which reduces need for "bridging" with a parenteral anticoagulant, that they don't require frequent monitoring or re-dosing whilst having few strong drug interactions and no food interactions, leading to greater convenience by patients and doctors and that they have a lower risk of intra cranial bleeding in trials.
Disadvantages compared to warfarin include the currently limited prospective experience, concerns regarding patient adherence without laboratory monitoring, uncertainty about dosing in some patient populations (e.g., renal dysfunction, marked extremes of body weight), their contraindication in severe renal impairment, their lack of specific antidotes and assays to measure drug levels in case of severe bleeding, their potential to overuse in low risk atrial fibrillation people, their short half live affecting efficacy and their higher drug acquisition costs.[2]
Antidotes
Specific antidotes to reverse the anticoagulant activity of direct Xa inhibitors and other direct oral anticoagulants (DOACs) in the event of major bleeding are not available. Evidence supporting non-specific prohemostatic therapies (prothrombin complex concentrate [PCC], activated prothrombin complex concentrate [aPCC], recombinant factor VIIa) in this setting is limited to healthy human volunteers, animal models, and in vitro studies. Clinical outcome data are lacking. Administration of PCC or aPCC may be considered in addition to supportive measures for patients with severe or life-threatening bleeding.[3] Recent studies are using recombinant proteins (r-Antidote) that are catalytically inactive and lack the membrane-binding γ-carboxyglutamic acid domain of native fXa but retain the ability of native fXa to bind direct fXa inhibitors as well as low molecular weight heparin-activated antithrombin III (ATIII). r-Antidote dose-dependently reverses the inhibition of fXa by direct fXa inhibitors and corrects the prolongation of ex vivo clotting times by such inhibitors. The r-antidote has the potential to be used as a universal antidote for a broad range of fXa inhibitors.[4]
Products
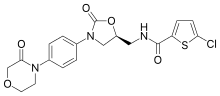
A new series of oral, direct-acting inhibitors of Factor Xa have entered clinical development, and are competitors of dabigatran, which is a direct thrombin (factor IIa) inhibitor. These include rivaroxaban (Xarelto) from Bayer, apixaban (Eliquis) from Bristol-Myers Squibb, betrixaban from Portola Pharmaceuticals, darexaban (YM150) from Astellas, edoxaban (Lixiana) from Daiichi,[5] otamixaban by Sanofi, and more recently letaxaban (TAK-442) from Takeda and eribaxaban (PD0348292) from Pfizer.
The development of darexaban was discontinued in September 2011: in a trial for prevention of recurrences of myocardial infarction in top of dual anti platelet therapy, the drug didn't work and the risk for bleeding was increased by 300%.[6]
The mechanism of action of these drugs can be easily recalled from the name. Ex: Rivaro(Identifier)-xa(FactorXa)-ban(inhibitor)
History
A naturally occurring inhibitor of factor Xa was first reported in 1971 by Spellman et al. from the dog hookworm. In 1987, Tuszynski et al. discovered antistasin, which was isolated from the extracts of Mexican leech, Haementeria officinalis. Soon after this, another naturally occurring inhibitor, tick anticoagulant peptide (TAP) was isolated from the extract of tick Ornithodoros moubata.[7]
References
- ↑ "Medscape.com". Retrieved 2009-01-23.
- 1 2 Bauer, K. A. (6 December 2013). "Pros and cons of new oral anticoagulants". Hematology. 2013 (1): 464–470. doi:10.1182/asheducation-2013.1.464.
- ↑ Siegal, D. M.; Cuker, A (2013). "Reversal of novel oral anticoagulants in patients with major bleeding". Journal of Thrombosis and Thrombolysis. 35 (3): 391–8. doi:10.1007/s11239-013-0885-0. PMID 23389753.
- ↑ Lu, G; Deguzman, F. R.; Hollenbach, S. J.; Karbarz, M. J.; Abe, K; Lee, G; Luan, P; Hutchaleelaha, A; Inagaki, M; Conley, P. B.; Phillips, D. R.; Sinha, U (2013). "A specific antidote for reversal of anticoagulation by direct and indirect inhibitors of coagulation factor Xa". Nature Medicine. 19 (4): 446–51. doi:10.1038/nm.3102. PMID 23455714.
- ↑ Turpie, AG (Jan 2008). "New oral anticoagulants in atrial fibrillation.". European Heart Journal. 29 (2): 155–65. doi:10.1093/eurheartj/ehm575. PMID 18096568.
- ↑ Grogan, Kevin (September 29, 2011). "Astellas pulls the plug on darexaban". Pharmatimes. Retrieved 11 April 2014.
- ↑ "P15358 antistasin". Uniprot. Retrieved 11 April 2014.
- Spellman, GG Jr.; Nossel, HL (1971). "Anticoagulant activity of dog hookworm". Am J Physiology. 222: 922–927.
External links
- Direct Factor Xa Inhibitors as Anticoagulants | PharmaXChange.info – A review and presentation on the available factor Xa inhibitors which can be used as anticoagulants.
- Oral Xa inhibitors – Literature review of the evidence regarding oral Xa inhibitors
- http://ajplegacy.physiology.org/content/220/4/922.full-text.pdf+html