Anterior cruciate ligament injury
| Anterior cruciate ligament injury | |
|---|---|
|
Diagram of the right knee | |
| Classification and external resources | |
| Specialty | Orthopedics |
| ICD-10 | S83.5 |
| ICD-9-CM | 844.2 |
| eMedicine | pmr/3 |
The anterior cruciate ligament (ACL) is an important internal stabilizer of the knee joint, restraining hyperextension. Anterior cruciate ligament injury occurs when the biomechanical limits of the ligament are exceeded (over-stretched), often with a hyperextension mechanism.
Formerly, ACL injuries occurred most often in a sports contact injury, when other structures were frequently involved. A severe form of the contact injury is called the "unhappy triad" or "O'Donaghue's triad", and involves the anterior cruciate ligament, the medial collateral ligament, and the medial meniscus. Presently, ACL injury is more commonly a non-contact injury, such as a dismount from a layup in basketball. Both forms occur more frequently in athletes than in the general population and are prevalent in alpine skiing, association football, American football, Australian rules football, basketball, rugby, professional wrestling, martial arts, and artistic gymnastics.[1] It is also known to be about three times more common in women than men.[1]
The consequences of the injury depend on how much the stability of the knee is affected, and the extent to which other structures have been involved, and this can vary on a case-by-case basis. If instability is evident, particularly rotatory instability, then the menisci will get injured, sooner or later, setting the scene for progressive, degenerative, arthritis of the knee.
Signs and symptoms
There is a "popping sound" during a twisting movement[2] or rapid deceleration, together with inability to continue participation, and followed by early swelling, is said to indicate a 90% probability of rupture of the anterior cruciate ligament.[3] An individual may experience instability in the knee once they resume walking and other activities.
Causes

ACL injuries occur when an individual stops suddenly or plants his or her foot hard into the ground (cutting). ACL failure has also been linked to heavy or stiff-legged landing; the knee rotating while landing, especially when the knee is in an unnatural position.
Women in sports such as association football, basketball, and tennis are significantly more prone to ACL injuries than men. The discrepancy has been attributed to gender differences in anatomy, general muscular strength, reaction time of muscle contraction and coordination, and training techniques. Women also have a relatively wider pelvis, requiring the femur to angle toward the knees. This angle towards the knee is referred to as the Q angle. The average Q angle for men is 14 degrees and the average for women is 17 degrees. Steps can be taken to reduce this Q angle, such as using orthotics.[4] The role of genetics is currently speculative.
Significantly many ACL injuries occur in athletes landing flat on their heels. The latter directs the forces directly up the tibia into the knee, while the straight-knee position places the anterior femoral condyle on the back-slanted portion of the tibia. The resultant forward slide of the tibia relative to the femur is restrained primarily by the now-vulnerable ACL.
Ligament dominance
The increased risk of anterior cruciate ligament injury among female athletes is best predicted by the motion and loading of the knee during performance situations.[5] The ligament dominance theory suggests that females typically perform athletic movements with greater knee valgus angles. A greater amount of stress is placed on the ACL in these situations because there is high activation of the quadriceps muscles despite limited knee flexion, limited hip flexion, greater hip adduction, and a large knee adductor moment.[6][7] Additionally, females typically land with their tibia rotated internally or externally.[8] As a result of increased knee valgus stress, ground reaction forces are greater and laterally directed.[9]
Quadriceps dominance
Ligament dominance is observed when there is excessive movement in the frontal plane to accommodate limited movement in the sagittal plane. This is caused by weakness in the hamstring muscles or reliance on the strength of the quadriceps muscles.[7] This quadriceps dominance theory identifies when the hamstring muscles are notably weaker than the quadriceps muscles. As a result, knee stability in performance situations depends on the quadriceps due to a discrepancy in the pattern in recruiting quadriceps and hamstring muscles.[10]
Trunk and leg dominance
Other theories used to explain the increased risk of ACL injury among female athletes include the trunk dominance and leg dominance theories. Trunk dominance suggests that males typically exhibit greater control of the trunk in performance situations as evidenced by greater activation of the internal oblique muscle. Leg dominance suggests that females exhibit greater kinematic leg asymmetry in knee valgus angles, hip abduction, and ankle abduction in performance situations.[6]
 |
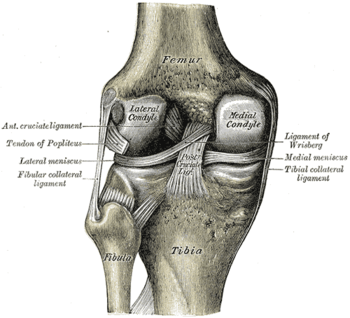 |
| Right knee, front, showing interior ligaments | Left knee, behind, showing interior ligaments |
Diagnosis

The pivot-shift test, anterior drawer test, and Lachman test are used during the clinical examination of suspected ACL injury. The Lachman test is recognized by most authorities as the most reliable and sensitive test, and usually superior to the anterior drawer test.[11] The ACL can also be visualized using a magnetic resonance imaging scan (MRI scan).
An ACL tear can present with a popping sound heard after impact, swelling after a couple of hours, severe pain when bending the knee, and buckling or locking of the knee during movement.
Though clinical examination in experienced hands can be accurate, the diagnosis is usually confirmed by MRI, which has greatly lessened the need for diagnostic arthroscopy and which has a higher accuracy than clinical examination. It may also permit visualization of other structures which may have been coincidentally involved, such as a meniscus, or collateral ligament, or posterolateral corner of the knee joint.
Prevention
Interest in reducing non-contact ACL injury has been intense and the observed, increased, liability of the female gender in some sports has added to this. The International Olympic Committee, after a comprehensive review of preventive strategies, has stated that injury prevention programs have an effect on reducing injuries that is measurable, and that applies particularly to women.[12] Further, paying attention to the balance of strength between hamstrings and quadriceps will help prevent the anterior cruciate ligament from being overpowered by over-emphasized quadriceps strength. It is also stressed that landing forces should be reduced together with emphasizing proper landing technique. It has been previously reported that landing on the heel, rather than forefoot with progressive transfer of weight to the heel, is potentially injurious to the ACL because of the hyperextension forces created. The closer the knee is to full extension, the more likely this is to occur.[13]
Accordingly, it is generally recommended that injury prevention programs stress these principles.
Treatment
The term for non-surgical treatment for ACL rupture is "conservative management", and it often includes physical therapy and using a knee brace. Instability associated with ACL deficiency increases the risk of other knee injuries such as a torn meniscus, so sports with cutting and twisting motions are problematic and surgery is often recommended in those circumstances.
Patients who have suffered an ACL injury should be evaluated for other injuries that often occur in combination with an ACL tear and include cartilage/meniscus injuries, bone bruises, PCL tears, posterolateral injuries and collateral ligament injuries.
Conservative
A torn ACL is less likely to restrict the movement of the knee. When tears to the ACL are not repaired it can sometimes cause damage to the cartilage inside the knee because with the torn ACL the tibia and femur bone are more likely to rub against each other. Immediately after the tear of the ACL, the person should rest the knee, ice it every 15 to 20 minutes, provide compression on the knee, and then elevate above the heart; this process helps decrease the swelling and reduce the pain. The form of treatment is determined based on the severity of the tear on the ligament. Small tears in the ACL may just require several months of rehab in order to strengthen the surrounding muscles, the hamstring and the quadriceps, so that these muscles can compensate for the torn ligament. Falls associated with knee instability may require the use of a specific brace to stabilize the knee. Women are more likely to experience falls associated with the knee giving way. Sudden falls can be associated with further complications such as fractures and head injury.
Surgery
If surgery is decided upon, either because obvious instability interferes with activities of daily living, or because the knee is subject to repeated, severe, provocative maneuvers, such as the case of the competitive athlete involved in cutting and rapid deceleration etc., then several issues need to be decided upon.
- Timing. Immediate repair is usually avoided and initial swelling and inflammatory reaction allowed to subside.
- Choice of graft material, autograft or allograft.
- Choice of anterior cruciate ligament augmentation, patellar tendon or hamstring tendon.[14]
These issues are fully explored at ACL Reconstruction,
Rehabilitation
Before undertaking ACL reconstruction, the patient must accept that rehabilitation is mandatory, not optional, is fatiguing and time-consuming, and will last at least six months, more likely twelve, before optimal function is regained. Initial rehabilitation emphasizes recovery of range of motion, the preferred modality being isometric exercise that does not place stress on the knee joint. One goal is the achievement of full knee extension after two weeks. Although a minimum of six weeks is required for bony consolidation of the graft, walking is generally permitted. Thereafter, increased strengthening along with flexibility takes place until the important twelve-week post surgical timeline, when a more aggressive regimen begins. Rehabilitation is not only recovery but protection against future injury and attention to quadriceps strength, and importantly, ratio of hamstring to quadriceps strength as previously mentioned, will be emphasized.
Rehabilitation and recovery are discussed in detail at ACL reconstruction.
Gender differences
Gender difference in ACL tears in relationship with physical activities have been asserted.[15] A review of NCAA data has found relative rates of injury per 1000 athlete exposures as follows:
- Men's basketball 0.07, women's basketball 0.23
- Men's lacrosse 0.12, women's lacrosse 0.17
- Men's football 0.09, women's football 0.28
The highest rate of ACL injury in women occurred in gymnastics, with a rate of injury per 1000 athlete exposures of 0.33 Of the four sports with the highest ACL injury rates, three were women's – gymnastics, basketball and soccer.[16]
According to recent studies, female athletes are two to eight times more likely to strain their anterior cruciate ligament (ACL) in sports that involve cutting and jumping as compared to men who play the same particular sports (soccer, basketball, and volleyball).[17] Differences between males and females identified as potential causes are the active muscular protection of the knee joint, the greater Q angle putting more medial torque on the knee joint, relative ligament laxity caused by differences in hormonal activity from estrogen and relaxin, intercondylar notch dimensions, and muscular strength.[17][18]
Hormonal Differences
Before puberty, there is no observed difference in frequency of ACL tears between the sexes. Changes in sex hormone levels, specifically elevated levels of estrogen and relaxin in females during the menstrual cycle, have been hypothesized as causing predisposition of ACL ruptures. This is because of how they increase joint laxity and extensibility of the soft tissues surrounding the knee joint.[17] Through the influence of sex hormones, female pelvises widen during puberty. The relatively wider female hip, which leads to an increased likelihood of ACL tears in women, thus stems from differences in sex hormones between males and females.
ACL, muscular stiffness, and strength
During puberty, sex hormones also affect the remodeled shape of soft tissues throughout the body. The tissue remodeling results in female ACLs that are smaller and will fail (i.e. tear) at lower loading forces, and differences in ligament and muscular stiffness between men and women. Women’s knees are less stiff than men’s during muscle activation. Force applied to a less stiff knee is more likely to result in ACL tears.[19]
In addition, the quadriceps femoris muscle is an antagonist to the ACL. According to a study done on female athletes at the University of Michigan, 31% of female athletes recruited the quadriceps femoris muscle first as compared to 17% in males. Because of the elevated contraction of the quadriceps femoris muscle during physical activity, an increased strain is placed onto the ACL due to the "tibial translation anteriorly".[20]
Special Populations
Young athletes
High school athletes are at increased risk for ACL tears when compared to non-athletes. This risk increases with certain types of sports. Among high school girls, the sport with the highest risk of ACL tear is soccer, followed by basketball and lacrosse. The highest risk sport for boys was football, followed by lacrosse and soccer.[21]
References
- 1 2 Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K (Dec 2007). "A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen". Arthroscopy. 23 (12): 1320–25. doi:10.1016/j.arthro.2007.07.003. PMID 18063176.
- ↑ "ACL Reconstruction Sydney NSW | ACL Injury Treatment Sydney NSW". Dr Stephen Rimmer | Sydney Orthopedic Knee Surgeon. 2016-10-16. Retrieved 2016-11-17.
- ↑ Bytomski J, Moorman C (2010). Oxford American Handbook of Sports Medicine. Oxford American Handbook of Medicine Series (First ed.). Oxford, New York: Oxford University Press. p. 290. ISBN 9780195372199.
- ↑ McLean SG, Huang X, van den Bogert AJ (2005). "Association between lower extremity posture at contact and peak when the tibia moves too far forward implications for ACL injury". Clin Biomech (Bristol, Avon). 20 (8): 863–70. doi:10.1016/j.clinbiomech.2005.05.007. PMID 16005555.
- ↑ Hewett T. E.; Myer G. D.; Ford K. R.; Heidt R. S.; Colosimo A. J.; McLean S. G.; den Bogert A. J.; Paterno M. V.; Succop P. (2005). "Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study". The American Journal of Sports Medicine. 33 (4): 492–501. doi:10.1177/0363546504269591.
- 1 2 Pappas E.; Carpes F. P. (2012). "Lower extremity kinematic asymmetry in male and female athletes performing jump-landing tasks". Journal of Science and Medicine in Sport. 15 (1): 87–92. doi:10.1016/j.jsams.2011.07.008.
- 1 2 Pollard C. D.; Sigward S. M.; Powers C. M. (2010). "Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments". Clinical Biomechanics. 25 (2): 142–146. doi:10.1016/j.clinbiomech.2009.10.005.
- ↑ Nagano Y.; Ida H.; Akai M.; Fukubayashi T. (2007). "Gender differences in knee kinematics and muscle activity during single limb drop landing". The Knee. 14 (3): 218–223. doi:10.1016/j.knee.2006.11.008.
- ↑ Sigward S. M.; Powers C. M. (2007). "Loading characteristics of females exhibiting excessive valgus moments during cutting". Clinical Biomechanics. 22 (7): 827–833. doi:10.1016/j.clinbiomech.2007.04.003.
- ↑ Ford K. R.; Myer G. D.; Hewett T. E. (2003). "Valgus knee motion during landing in high school female and male basketball players". Medicine and Science in Sports and Exercise. 31 (10): 1745–1750.
- ↑ van Eck CF, van den Bekerom MP, Fu FH, Poolman RW, Kerkhoffs GM (Aug 2013). "Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia". Knee Surg Sports Traumatol Arthrosc. 21 (8): 1895–903. doi:10.1007/s00167-012-2250-9. PMID 23085822.
- ↑ P Renstrom; A Ljungqvist; E Arendt; B Beynnon; T Fukubayashi; W Garrett; T Georgoulis; T E Hewett; R Johnson; T Krosshaug; B Mandelbaum; L Micheli; G Myklebust; E Roos; H Roos; P Schamasch; S Shultz; S Werner; E Wojtys; L Engebretsen (June 2008). "Non-contact ACL injuries in female athletes: an International Olympic Committee current concepts statement". Br J Sports Med. 42 (6): 394–412. doi:10.1136/bjsm.2008.048934. PMC 3920910
 . PMID 18539658.
. PMID 18539658. - ↑ Boden BP, Sheehan FT, Torg JS, Hewett TE (Sep 2010). "Non-contact ACL Injuries: Mechanisms and Risk Factors". J Am Acad Orthop Surg. 18 (9): 520–27. PMC 3625971
 . PMID 20810933.
. PMID 20810933. - ↑ Mohtadi, NG; Chan, DS; Dainty, KN; Whelan, DB (Sep 7, 2011). "Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults.". Cochrane Database of Systematic Reviews. 9 (9): CD005960. doi:10.1002/14651858.CD005960.pub2. PMID 21901700.
- ↑ Mountcastle SB, Posner M, Kragh JF, Taylor DC (October 2007). "Gender differences in anterior cruciate ligament injury vary with activity: epidemiology of anterior cruciate ligament injuries in a young, athletic population". Am J Sports Med. 35 (10): 1635–42. doi:10.1177/0363546507302917. PMID 17519438.
- ↑ Hootman JM, Dick R, Agel J (Apr–Jun 2007). "Epidemiology of Collegiate Injuries for 15 Sports: Summary and Recommendations for Injury Prevention Initiatives". J Athl Train. 42 (2): 311–19. PMC 1941297
 . PMID 17710181.
. PMID 17710181. - 1 2 3 Faryniarz, Deborah A.; Bhargava, Madhu; Lajam, Claudette; Attia, Erik T.; Hannafin, Jo A. (2006-07-01). "Quantitation of Estrogen Receptors and Relaxin Binding in Human Anterior Cruciate Ligament Fibroblasts". In Vitro Cellular & Developmental Biology. Animal. 42 (7): 176–181. JSTOR 4295693.
- ↑ Wojyts, Edward M., Laura J. Huston, Harold J. Schock, James P. Boylan, and James A. Ashton-Miller. "GENDER DIFFERENCES IN MUSCULAR PROTECTION OF THE KNEE IN TORSION IN SIZE-MATCHED ATHLETES." Journal of Bone & Joint Surgery 85.5 (2003): 782.EBSCOHost. Web. 2 Dec. 2015. <http://connection.ebscohost.com/c/articles/10013241/gender-differences-muscular-protection-knee-torsion-size-matched-athletes>.
- ↑ Slauterbeck, JR; Hickox JR; Beynnon B; Hardy DM (2006). "Anterior Cruciate Ligament Biology andIts Relationship to Injury Forces". Orthop Clin N Am. 37: 585–591. doi:10.1016/j.ocl.2006.09.001.
- ↑ Biondino, Robert (November 1999). "Anterior Cruciate Ligament Injuries in Female Athletes". Connecticut Medicine. 63 (11): 657–660. PMID 10589146.
- ↑ Gornitzky, Alex L.; Lott, Ariana; Yellin, Joseph L.; Fabricant, Peter D.; Lawrence, J. Todd; Ganley, Theodore J. (2016-10-01). "Sport-Specific Yearly Risk and Incidence of Anterior Cruciate Ligament Tears in High School Athletes: A Systematic Review and Meta-analysis". The American Journal of Sports Medicine. 44 (10): 2716–2723. doi:10.1177/0363546515617742. ISSN 1552-3365. PMID 26657853.

