Steatocystoma multiplex
| Steatocystoma multiplex | |
|---|---|
|
| |
| Classification and external resources | |
| Specialty | dermatology |
| ICD-10 | L72.2 |
| ICD-9-CM | 706.2 |
| OMIM | 184500 |
| DiseasesDB | 29808 |
| eMedicine | derm/404 |
Steatocystoma multiplex, also known as epidermal polycystic disease and sebocystomatosis,[1]:781 is a benign, autosomal dominant congenital condition resulting in multiple cysts on a person's body.
First described by Jamieson in 1873, and coined by Pringle in 1899, steatocystoma multiplex (SM) is an uncommon disorder of the pilosebaceous unit characterized by the development of numerous sebum-containing dermal cysts. Although steatocystoma multiplex has historically been described as an autosomal dominant inherited disorder, most presenting cases are sporadic. Steatocystoma simplex is the sporadic solitary tumor counterpart to steatocystoma multiplex.[2]
Causes and genetics
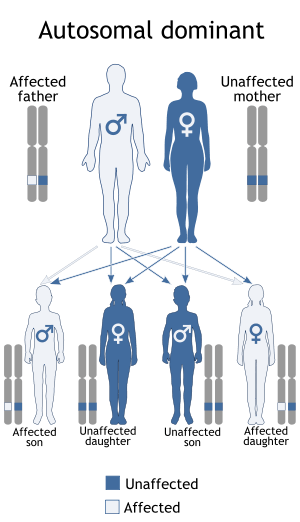
It is associated with defects in Keratin 17.[3] The condition is inherited in an autosomal dominant manner. This indicates that the defective gene responsible for a disorder is located on an autosome, and only one copy of the defective gene is sufficient to cause the disorder, when inherited from a parent who has the disorder.
However, a solitary case can also emerge in a family with no prior history of the disorder due to the occurrence of a new mutation (often referred to as a sporadic or spontaneous mutation).
Steatocystoma multiplex occurs as either a sporadic or autosomal dominant inherited condition characterized by benign sebaceous gland tumors. Lesions consist of a nevoid formation of abortive hair follicles at the site where sebaceous glands attach. Electron microscopy studies demonstrate cyst wall cells undergoing trichilemmal keratinization similar to that of the isthmus portion of the outer hair sheath. The relationship of steatocystoma multiplex to the development of sebaceous glands and common presentation at puberty suggest a hormonal trigger for lesion growth.
In the familial form of steatocystoma multiplex, mutations are localized to the keratin 17 (K17) gene in areas identical to mutations found in patients with pachyonychia congenita type 2 (PC-2). Pachyonychia congenita type 2, an autosomal dominant inherited disorder, is characterized by hypertrophic nail dystrophy, focal keratoderma, multiple pilosebaceous cysts, and a variety of conditions associated with ectodermal dysplasia. Keratin 17 is expressed in several epithelial structures, most notably in sebaceous glands, the outer root sheath of hair follicles, and the nail bed; its expression correlates well to the clinical phenotypic expression of both steatocystoma multiplex and pachyonychia congenita type 2. To date, 14 mutations have been described in patients with either steatocystoma multiplex or pachyonychia congenita type 2, all of which are localized to the helix initiation domain (1A domain) of the K17 gene.
Some authors propose that steatocystoma multiplex is simply a variant of pachyonychia congenita type 2 because they both share the same underlying etiology. Sporadic forms of steatocystoma multiplex have not been shown to be associated with K17 mutations. In previous reports, specific mutations were attributed to early-onset cyst formation in pachyonychia congenita type 2 and steatocystoma multiplex; however, more recent reports suggest that the age of onset is multifactorial.
Steatocystoma multiplex is often associated with eruptive vellus hair cysts (EVHCs). Both diseases share overlapping clinical features, including age of onset, location, appearance of lesions, and mode of inheritance. Reports of hybrid lesions showing histological features of both steatocystoma multiplex and eruptive vellus hair cysts exist. Given these similarities, some postulate that steatocystoma multiplex and eruptive vellus hair cysts are, in fact, variants of the same disease. However, major differences in keratin expression patterns between steatocystoma multiplex and eruptive vellus hair cysts have been elucidated, leading others to believe that they are 2 distinct disease entities. In steatocystoma multiplex associated with eruptive vellus hair cyst, no K17 mutation has been found.[2]
Treatment
The cysts can be moved via excision, though conventional cyst excision techniques have proven impractical, and a specialized regimen is required.[4]
Medical treatments have been used with variable results to lessen inflammation, minimize scarring, and reduce the need for surgery.
Steatocystoma suppurativa: Treatment is indicated for this scarring inflammatory version of the disorder and involves antimicrobial therapy in combination with incision and drainage. The classic treatment is with the tetracycline class of antibiotics. Isotretinoin therapy has been effective in some patients; however, in others, it has caused the condition to flare. Recurrence following isotretinoin treatment has been reported.
Disfiguring lesions: The patient may require medical intervention for significantly deforming lesions when surgical approaches are impractical. Unfortunately, isotretinoin (despite its known effect of decreasing sebaceous gland activity) has shown inconsistent results. Flaring and recurrence following isotretinoin have been reported.
Cysts can be widespread and difficult to treat. A variety of surgical treatment options have been used in the treatment of steatocystoma multiplex.
Cryosurgery: Cryosurgery has been used in the past with limited success. Residual scarring limits this approach.
Aspiration: Simple aspiration with 18-gauge needle has been successful in minimizing scarring of facial lesions, although a high rate of recurrence has been observed. Variation of this method by insertion and gentle extirpation of cystic contents without removing the cyst wall has been shown to be successful, with no scarring and a low rate of recurrence. This technique is thought to be the treatment of choice in the management of facial lesions and those smaller than 1.5 cm in diameter. This approach may not be feasible with larger, more mature lesions with cyst contents of a more dense consistency.
Surgical excision: Traditionally, surgical excision is the most commonly mentioned method of treatment. Excisional surgery with elliptical excisions, flaps, or grafts is often impractical for widespread lesions and has fallen out of favor secondary to its time-consuming nature and the associated risk of scarring. Punch excision followed by cyst removal has been used in the past, with mixed results.
Incisional variants: Incisional variants of cyst removal have become the preferred methods of treatment. Mini-incisions of 1 mm with a No. 11 surgical blade followed by expression of cyst contents and excochleation of the cyst wall using a 1-mm curette resulted in minimal scarring and a low rate of recurrence. A modified surgical technique, used on more than 50 lesions, is sharp-tipped cautery followed by expression of cyst contents and forceps-assisted removal of the cyst wall. This technique resulted in minimal depressed scarring and slight hypopigmentation with no evidence of recurrence. Newer techniques with small incisions, 2–3 mm in length, followed by removal of the cyst wall with a phlebectomy hook resulted in satisfactory cosmesis, with no recurrence noted.
Carbon dioxide laser: Carbon dioxide laser ablation has allowed treatment of multiple lesions during a single treatment session, with no anesthesia, a low percentage of recurrence, and good aesthetic results.[5]
See also
- Keratin disease
- Steatocystoma simplex
- List of cutaneous conditions
- List of cutaneous conditions caused by mutations in keratins
References
- ↑ Freedberg, et al. (2003). Fitzpatrick's Dermatology in General Medicine. (6th ed.). McGraw-Hill. ISBN 0-07-138076-0.
- 1 2 Davey, Mathew. "Steatocystoma Multiplex". Retrieved 25 May 2011.
- ↑ Smith FJ, Corden LD, Rugg EL, et al. (1997). "Missense mutations in keratin 17 cause either pachyonychia congenita type 2 or a phenotype resembling steatocystoma multiplex". J. Invest. Dermatol. 108 (2): 220–3. doi:10.1111/1523-1747.ep12335315. PMID 9008238.
- ↑ Pamoukian VN, Westreich M (1997). "Five generations with steatocystoma multiplex congenita: a treatment regimen". Plast. Reconstr. Surg. 99 (4): 1142–6. doi:10.1097/00006534-199704000-00036. PMID 9091916.
- ↑ Davey, Mathew. "Steatocystoma Multiplex". Retrieved 25 May 2011.