Surgery for benign prostatic hyperplasia
If medical treatment is not effective a person with benign prostatic hyperplasia may try office-based therapies or transurethral resection of prostate (TURP), surgery may need to be performed. Surgical techniques used include
- Open prostatectomy: not usually performed nowadays, even if results are very good.
- Trans-urethral resection of the prostate (TURP): the gold standard.
- Transurethral incision of the prostate (TUIP): rarely performed; the technique is similar to TURP but less definitive.
- Laser vaporization of the prostate: common treatment.
- Transurethral microwave therapy (TUMT): similar to laser ablation, but less effective and much less used.
- Transurethral needle ablation (TUNA): not very effective.
- Holmium laser enucleation of the prostate (HoLEP): more and more used, it will probably replace TURP in the future.
In general, TURP is still considered the gold standard of prostate interventions for people who require a procedure. This involves removing (part of) the prostate through the urethra. However, after this endoscopic surgery the ejaculations are dry and the person becomes sterile. For a man who wishes to father a child this is not the procedure of choice. Over the past couple of decades efforts to find newer surgical methods have resulted in newer approaches and different types of energies being used to treat the enlarged gland. However some of the newer methods for reducing the size of an enlarged prostate, have not been around long enough to fully establish their safety or side-effects. These include various methods to destroy or remove part of the excess tissue while trying to avoid damaging what remains. Transurethral electrovaporization of the prostate (TVP), laser TURP, visual laser ablation (VLAP), ethanol injection, and others are studied as alternatives.
Newer techniques involving lasers in urology have emerged in the last 5–10 years, starting with the VLAP technique involving the Nd:YAG laser with contact on the prostatic tissue. A similar technology called photoselective vaporization of the prostate (PVP) with the GreenLight (KTP or LBO crystal) laser have emerged very recently. This procedure involves a high-power 180-watt 532 nm wavelength laser with a 650-micrometre laser fiber inserted into the prostate. This fiber has an internal reflection with a 70-degree deflecting angle. It is used to vaporize the tissue to the prostatic capsule. GreenLight 532 nm lasers target haemoglobin as the chromophore and typically have a penetration depth of 0.8 mm (twice as deep as holmium). The procedure termed Holmium Laser Ablation of the Prostate (HoLAP) has been gaining acceptance around the world. Like KTP, the delivery device for HoLAP procedures is a 550 um disposable side-firing fiber that directs the beam from a high-power 100-watt laser at a 70-degree angle from the fiber axis. The holmium wavelength is 2,140 nm, which falls within the infrared portion of the spectrum and is invisible to the naked eye. Whereas GreenLight relies on haemoglobin as a chromophore, water within the target tissue is the chromophore for Holmium lasers. The penetration depth of Holmium lasers is <0.4 mm, avoiding complications associated with tissue necrosis often found with the deeper penetration and lower peak powers of Nd:YAG lasers used in the 1990s.
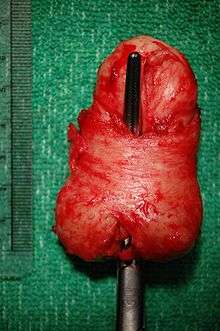
HoLEP, Holmium Laser Enucleation of the Prostate, is another Holmium laser procedure reported to carry fewer risks compared with either TURP or open prostatectomy.[1] HoLEP is largely similar to the HoLAP procedure; the main difference is that this procedure is typically performed on larger prostates. Instead of ablating the tissue, the laser cuts a portion of the prostate, which is then cut into smaller pieces and flushed with irrigation fluid. As with the HoLAP procedure, there is little bleeding during or after the procedure. A 2015 review concludes that HoLEP is superior to TURP and should become the new gold standard.[2]
Both wavelengths, GreenLight and Holmium, ablate approximately one to two grams of tissue per minute.
Post-surgical care often involves placement of a Foley catheter or a temporary prostatic stent to permit healing and allow urine to drain from the bladder.
Minimally invasive therapies
Many people do not achieve success with medication. They may not achieve sustained improvement in symptoms or may stop taking the medication because of side-effects.[3] There are options for treatment in a urologist's office before proceeding to surgery. The two most common types of office-based therapies are transurethral microwave thermotherapy (TUMT) and transurethral needle ablation (TUNA). Both of these procedures rely on delivering enough energy to create sufficient heat to cause cell death (necrosis) in the prostate. The goal is to cause enough necrosis so that, when the dead tissue is reabsorbed by the body, the prostate shrinks, relieving the obstruction of the urethra. These procedures are typically performed with local anesthesia, and the patient returns home the same day. Some urologists have studied and published long-term data on the outcomes of these procedures, with data out to five years. The most recent American Urological Association (AUA) Guidelines for the Treatment of BPH in 2003 lists minimally invasive therapies including TUMT and TUNA as acceptable alternatives for certain patients with BPH.[4] However, European guidelines do not recommend the use of TUMT or TUNA over surgery.[5]
Transurethral microwave thermotherapy (TUMT) was originally approved by the United States Food and Drug Administration (FDA) in 1996, with the first generation system by EDAP Technomed. Since 1996, other companies have received FDA approval for TUMT devices, including Urologix, Dornier, Thermatrix, Celsion, and Prostalund. Multiple clinical studies have been published on TUMT. The general principle underlying all the devices is that a microwave antenna that resides in a urethral catheter is placed in the intraprostatic area of the urethra. The catheter is connected to a control box outside of the patient's body and is energized to emit microwave radiation into the prostate to heat the tissue and cause necrosis. It is a one-time treatment that takes approximately 30 minutes to 1 hour, depending on the system used. It takes approximately 4 to 6 weeks for the damaged tissue to be reabsorbed into the patient's body. Some of the devices incorporate circulating coolant through the treatment area with the intent of preserving the urethra while the microwave energy heats the prostatic tissue surrounding the urethra.
Transurethral needle ablation (TUNA) operates with a different type of energy, radio frequency (RF) energy, but is designed along the same premise as TUMT devices, that the heat the device generates will cause necrosis of the prostatic tissue and shrink the prostate. The TUNA device is inserted into the urethra using a rigid scope much like a cystoscope. The energy is delivered into the prostate using two needles that emerge from the sides of the device, through the urethral wall and into the prostate. The needle-based ablation devices are very effective at heating a localized area to a high enough temperature to cause necrosis. The treatment is typically performed in one session, but may require multiple sticks of the needles depending on the size of the prostate.
In 2013 the US FDA approved the UroLift device/procedure of transurethrally placed sutures.[6]
References
- ↑ Gilling, Peter J.; Aho, Tevita F.; Frampton, Christopher M.; King, Colleen J.; Fraundorfer, Mark R. (2008). "Holmium Laser Enucleation of the Prostate: Results at 6 Years". European Urology. 53 (4): 744–9. doi:10.1016/j.eururo.2007.04.052. PMID 17475395.
- ↑ Michalak, J; Tzou, D; Funk, J (2015). "HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century.". American journal of clinical and experimental urology. 3 (1): 36–42. PMID 26069886.
- ↑ Roehrborn, CG (2008). "Current Medical Therapies for Men With Lower Urinary Tract Symptoms and Benign Prostatic Hyperplasia: Achievements and Limitations". Reviews in urology. 10 (1): 14–25. PMC 2312341
 . PMID 18470272.
. PMID 18470272. - ↑ AUA Clinical guidelines for management of BPH
- ↑ "Interventional procedure overview of insertion of prostatic urethral lift implants to treat lower urinary tract symptoms secondary to benign prostatic hyperplasia". NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE.
- ↑ FDA Approves Device to Treat Enlarged Prostate. Sept 2013