3,4-Methylenedioxyamphetamine
 | |
 | |
| Clinical data | |
|---|---|
| Routes of administration | Oral, Sublingual, Insufflation |
| ATC code | None |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Metabolism | Hepatic, CYP extensively involved |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number |
4764-17-4 |
| PubChem (CID) | 1614 |
| DrugBank |
DB01509 |
| ChemSpider |
1555 |
| UNII |
XJZ28FJ27W |
| ChEMBL |
CHEMBL6731 |
| Chemical and physical data | |
| Formula | C10H13NO2 |
| Molar mass | 179.22 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
3,4-Methylenedioxyamphetamine (MDA), also known as tenamfetamine (INN), is a psychoactive drug of the substituted methylenedioxyphenethylamine and substituted amphetamine classes of drugs that is consumed primarily for its entactogenic, psychedelic, and psychostimulant effects. Pharmacologically, MDA acts as a serotonin-norepinephrine-dopamine releasing agent and reuptake inhibitor. Possession of MDA is illegal in most countries. Some limited exceptions exist for scientific and medical research in few countries. The recreational use of MDA predates its more widely used analog MDMA (ecstasy).
Use
Medical
MDA currently has no accepted medical use.
Recreational
Although illegal, MDA is bought, sold, and used as a recreational 'love drug', due to its enhancement of empathy.[1] A recreational dose of MDA is commonly between 100 and 160 mg.[2]
Overdose
Symptoms of acute toxicity may include agitation, sweating, increased blood pressure and heart rate, dramatic increase in body temperature, convulsions, and death. Death is usually caused by cardiac effects and subsequent hemorrhaging in the brain (stroke).[3]
Pharmacology
Pharmacodynamics
MDA is a substrate of the serotonin, norepinephrine, and dopamine transporters, as well as a TAAR1 agonist,[4][5] and for that reason, acts as a reuptake inhibitor and releasing agent of serotonin, norepinephrine, and dopamine (or as an SNDRA).[6] It is also an agonist of the 5-HT2A,[7] 5-HT2B,[8] and 5-HT2C receptors,[9] and shows affinity for the α2A-, α2B-, α2C-adrenergic receptors and 5-HT1A and 5-HT7 receptors.[10]
The effect on serotonin may explain the similar entactogenic effects of MDMA and MDA. However, (S)-MDA has a higher efficacy in agonizing the 5-HT2A receptor than (R)-MDMA; thus MDA tends to cause more psychedelic-like effects, such as visual hallucinations. MDMA can also produce psychedelic-like visual effects, though these are generally less pronounced than those of MDA or require higher doses to become apparent. Relative to MDMA, MDA is also a more potent releasing agent of norepinephrine and dopamine and hence is more stimulating in comparison, and is also notably several-fold more neurotoxic to serotonergic neurons.
Pharmacokinetics
The (S)-optical isomer of MDA is more potent than the (R)-optical isomer as a psychostimulant, possessing greater affinity for the three monoamine transporter proteins (SERT, NET and DAT). The duration of the drug has been reported as about 6 to 8 hours.[2]
Chemistry
Synthesis
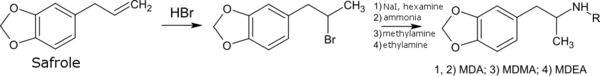
MDA is typically synthesized from essential oils such as safrole or piperonal. Common approaches from these precursors include:
- Reaction of safrole's alkene functional group with a Halogen containing mineral acid followed by Amine alkylation.[11][12]
- Wacker oxidation of safrole to yield 3,4-methylenedioxyphenylpropan-2-one (MDP2P) followed by reductive amination[12][13] or via reduction of its oxime.[14]
- Henry reaction of piperonal with nitroethane followed by nitro compound reduction.[12][15][16][17][18]
Detection in body fluids
MDA may be quantitated in blood, plasma or urine to monitor for use, confirm a diagnosis of poisoning or assist in the forensic investigation of a traffic or other criminal violation or a sudden death. Some drug abuse screening programs rely on hair, saliva, or sweat as specimens. Most commercial amphetamine immunoassay screening tests cross-react significantly with MDA and major metabolites of MDMA, but chromatographic techniques can easily distinguish and separately measure each of these substances. The concentrations of MDA in the blood or urine of a person who has taken only MDMA are, in general, less than 10% those of the parent drug.[19][20][21]
History
MDA was first synthesized by C. Mannich and W. Jacobsohn in 1910.[14] It was first ingested in July 1930 by Gordon Alles who later licensed the drug to Smith, Kline & French.[22] MDA was first used in animal tests in 1939, and human trials began in 1941 in the exploration of possible therapies for Parkinson's disease. From 1949 to 1957, more than 500 human subjects were given MDA in an investigation of its potential use as an antidepressant and/or anorectic by Smith, Kline & French. The United States Army also experimented with the drug, code named EA-1298, while working to develop a truth drug or incapacitating agent. Harold Blauer[23] died in January 1953 after being intravenously injected with 450 mg of the drug. MDA was patented as a cough suppressant by H. D. Brown in 1958, as an ataractic by Smith, Kline & French in 1960, and as an anorectic under the trade name "Amphedoxamine" in 1961. MDA began to appear on the recreational drug scene around 1963 to 1964. It was then inexpensive and readily available as a research chemical from several scientific supply houses. Several researchers, including Claudio Naranjo and Richard Yensen, have explored MDA in the field of psychotherapy.[24][25]
Legal Status
Australia
MDA is schedule 9 prohibited substance under the Poisons Standards.[26] A schedule 9 substance is listed as a "Substances which may be abused or misused, the manufacture, possession, sale or use of which should be prohibited by law except when required for medical or scientific research, or for analytical, teaching or training purposes with approval of Commonwealth and/or State or Territory Health Authorities."[26]
United States
MDA is a schedule 1 controlled substance in the US.
Research
In 2010, Matthew Baggott and colleagues studied the ability of MDA to invoke mystical experiences and alter vision in healthy volunteers.[27]
Derivatives
Tenamfetamine also constitutes part of the core structure of the LABA Protokylol.
References
- ↑ Monte AP, Marona-Lewicka D, Cozzi NV, Nichols DE (1993). "Synthesis and pharmacological examination of benzofuran, indan, and tetralin analogues of 3,4-(methylenedioxy)amphetamine". Journal of Medicinal Chemistry. 36 (23): 3700–3706. doi:10.1021/jm00075a027. PMID 8246240.
- 1 2 Baggott, MJ; Siegrist, JD; Galloway, GP; Robertson, LC; Coyle, JR; Mendelson, JE. "Investigating the Mechanisms of Hallucinogen-Induced Visions Using 3,4-Methylenedioxeamphetamine (MDA): A Randomized Controlled Trial in Humans". PLOS ONE. 5: e14074. doi:10.1371/journal.pone.0014074.
- ↑ Diaz, Jaime. How Drugs Influence Behavior. Englewood Cliffs: Prentice Hall, 1996.
- ↑ Lewin AH, Miller GM, Gilmour B (December 2011). "Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class". Bioorg. Med. Chem. 19 (23): 7044–8. doi:10.1016/j.bmc.2011.10.007. PMC 3236098
 . PMID 22037049.
. PMID 22037049. - ↑ Wallach, J.V. (2009). "Endogenous hallucinogens as ligands of the trace amine receptors: A possible role in sensory perception". Medical Hypotheses. 72 (1): 91–94. doi:10.1016/j.mehy.2008.07.052. ISSN 0306-9877. PMID 18805646.
- ↑ Rothman RB, Baumann MH (2006). "Therapeutic potential of monoamine transporter substrates". Curr Top Med Chem. 6 (17): 1845–59. doi:10.2174/156802606778249766. PMID 17017961.
- ↑ Giuseppe Di Giovanni; Vincenzo Di Matteo; Ennio Esposito (2008). Serotonin-dopamine Interaction: Experimental Evidence and Therapeutic Relevance. Elsevier. pp. 294–. ISBN 978-0-444-53235-0.
- ↑ Rothman, Richard B; Baumann, Michael H (2009). "Serotonergic drugs and valvular heart disease". Expert Opinion on Drug Safety. 8 (3): 317–329. doi:10.1517/14740330902931524. ISSN 1474-0338. PMC 2695569
 . PMID 19505264.
. PMID 19505264. - ↑ Nash JF, Roth BL, Brodkin JD, Nichols DE, Gudelsky GA (1994). "Effect of the R(-) and S(+) isomers of MDA and MDMA on phosphatidyl inositol turnover in cultured cells expressing 5-HT2A or 5-HT2C receptors". Neurosci. Lett. 177 (1–2): 111–5. doi:10.1016/0304-3940(94)90057-4. PMID 7824160.
- ↑ Manzoni, Olivier Jacques; Ray, Thomas S. (2010). "Psychedelics and the Human Receptorome". PLoS ONE. 5 (2): e9019. doi:10.1371/journal.pone.0009019. ISSN 1932-6203. PMC 2814854
 . PMID 20126400.
. PMID 20126400. - ↑ Muszynski, I.E. (1961). "Production of some amphetamine derivatives". Acta poloniae pharmaceutica. 18: 471–478. PMID 14477621.
- 1 2 3 Shulgin, Alexander; Manning, Tania; Daley, Paul (2011). The Shulgin Index, Volume One: Psychedelic Phenethylamines and Related Compounds (1st ed.). Berkeley, CA: Transform Press. p. 165. ISBN 9780963009630.
- ↑ Noggle, FT Jr; DeRuiter, J.; Long, MJ. (1986). "Spectrophotometric and liquid chromatographic identification of 3,4-methylenedioxyphenylisopropylamine and its N-methyl and N-ethyl homologs". Journal Association of Official Analytical Chemists. 69 (4): 681–686. PMID 2875058.
- 1 2 Mannich, C.; Jacobsohn, W.; Mannich, Hr. C. (1910). "Über Oxyphenyl-alkylamine und Dioxyphenyl-alkylamine". Berichte der deutschen chemischen Gesellschaft. 41 (1): 189–197. doi:10.1002/cber.19100430126.
- ↑ Ho, Beng-Thong; McIsaac, William M.; An, Rong; Tansey, L. Wayne; Walker, Kenneth E.; Englert Jr., Leo F.; Noel, Michael B. (1970). "Analogs of a-methylphenethylamine". Journal of Medicinal Chemistry. 13 (1): 26–30. doi:10.1021/jm00295a007. PMID 5412110.
- ↑ Butterick, John R.; Unrau, A. M. (1974). "Reduction of β-nitrostyrene with sodium bis-(2-methoxyethoxy)-aluminium dihydride. A convenient route to substituted phenylisopropylamines". Journal of the Chemical Society, Chemical Communications. 8 (8): 307–308. doi:10.1039/C39740000307.
- ↑ Toshitaka, Ohshita; Hiroaka, Ando (1992). "Synthesis of Phenethylamine Derivatives as Hallucinogen" (PDF). Japanese Journal of Toxicology and Environmental Health. 38 (6): 571–580. Retrieved 20 June 2014.
- ↑ Shulgin, Alexander & Shulgin, Ann (1991). PiHKAL: A Chemical Love Story. Lafayette, CA: Transform Press. ISBN 9780963009609.
- ↑ Kolbrich EA, Goodwin RS, Gorelick DA, Hayes RJ, Stein EA, Huestis MA. Plasma pharmacokinetics of 3,4-methylenedioxymethamphetamine after controlled oral administration to young adults. Ther. Drug Monit. 30: 320–332, 2008.
- ↑ Barnes AJ, De Martinis BS, Gorelick DA, Goodwin RS, Kolbrich EA, Huestis MA (2009). "Disposition of MDMA and metabolites in human sweat following controlled MDMA administration" (PDF). Clinical Chemistry. 55 (3): 454–62. doi:10.1373/clinchem.2008.117093. PMC 2669283
 . PMID 19168553.
. PMID 19168553. - ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 9th edition, Biomedical Publications, Seal Beach, California, 2011, pp. 1078–1080.
- ↑ The First MDA trip and the measurement of ‘mystical experience’ after MDA, LSD, and Psilocybin http://psychedelicresearch.org/?p=45
- ↑ The History Channel documented details of his death here https://www.youtube.com/watch?v=ySw-0uY4CUA See minute 2:38 onward.
- ↑ Naranjo, C.; Shulgin, A. T.; Sargent, T. (1967). "Evaluation of 3, 4-methylenedioxeamphetamine (MDA) as an adjunct to psychotherapy". Pharmacology. 17 (4): 359–364. doi:10.1159/000137100.
- ↑ Yensen, R.; Di Leo, F. B.; Rhead, J. C.; Richards, W. A.; Soskin, R. A.; Turek, B.; Kurland, A. A. (1976). "MDA-assisted psychotherapy with neurotic outpatients: a pilot study". The Journal of Nervous and Mental Disease. 163 (4): 233–245. doi:10.1097/00005053-197610000-00002. PMID 972325.
- 1 2 Poisons Standard (October 2015) https://www.comlaw.gov.au/Details/F2015L01534/Html/Text#_Toc420496379
- ↑ Baggott, M. J.; Siegrist, J. D.; Galloway, G. P.; Robertson, L. C.; Coyle, J. R.; Mendelson, J. E. (2010). "Investigating the mechanisms of hallucinogen-induced visions using 3, 4-methylenedioxeamphetamine (MDA): a randomized controlled trial in humans". PLOS ONE. 5 (12): e14074. doi:10.1371/journal.pone.0014074.