Sickle cell trait
| Sickle cell trait | |
|---|---|
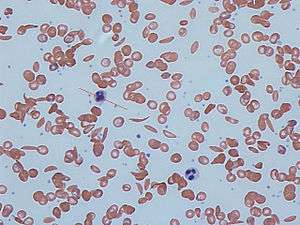 | |
| Sickle cells in human blood: both normal red blood cells and sickle-shaped cells are present | |
| Classification and external resources | |
| Specialty | hematology |
| ICD-10 | D57.3 |
| ICD-9-CM | 282.5 |
| OMIM | 603903 |
| MedlinePlus | 000527 |
| eMedicine | topic list |
| MeSH | D012805 |
Sickle cell trait (or sicklemia) describes a condition in which a person has one abnormal allele of the hemoglobin beta gene (is heterozygous), but does not display the severe symptoms of sickle cell disease that occur in a person who has two copies of that allele (is homozygous). Those who are heterozygous for the sickle cell allele produce both normal and abnormal hemoglobin (the two alleles are codominant with respect to the actual concentration of hemoglobin in the circulating cells).
Sickle cell disease is a blood disorder in which there is a single amino acid substitution in the hemoglobin protein of the red blood cells, which causes these cells to assume a sickle shape, especially when under low oxygen tension. Sickling and sickle cell disease also confer some resistance to malaria parasitization of red blood cells, so that individuals with sickle-cell trait (heterozygotes) have a selective advantage in environments where malaria is present.
Hemoglobin genetics
Normally, a person inherits two copies of the gene that produces beta-globin, a protein needed to produce normal hemoglobin (hemoglobin A, genotype AA). A person with sickle cell trait inherits one normal allele and one abnormal allele encoding hemoglobin S (hemoglobin genotype AS).
The sickle cell trait can be used to demonstrate the concepts of co-dominance and incomplete dominance. An individual with the sickle cell trait shows incomplete dominance when the shape of the red blood cell is considered. This is because the sickling happens only at low oxygen concentrations. With regards to the actual concentration of hemoglobin in the circulating cells, the alleles demonstrate co-dominance as both 'normal' and mutant forms co-exist in the blood stream. It is interesting to note that unlike the sickle-cell trait, sickle cell disease is passed on in a recessive manner.[1]
The sickle cell gene has five haplotypes, which are named after its core geographical areas of distribution: Bantu, Benin, Cameroon, Senegalese and Saudi-Indian.[2]
Prevalence

Sickle cell trait prevalence is highest in West Africa, where it is found in 25% of the population. The trait also has a high prevalence in South and Central Americans, especially those in Panama. However, it also very infrequently appears in Mediterranean countries such as Italy, Greece, and Spain, where it most likely expanded via the selective pressure of malaria, a disease that was endemic to the region.[3]
Symptoms
Sickle cell trait is a hemoglobin genotype AS and is generally regarded as a benign condition.[4] However, individuals with sickle cell trait may have rare complications. For example, in November 2010, Dr. Jeffery K. Taubenberger of the National Institutes of Health discovered the earliest proof of sickle-cell disease while looking for the virus of the 1918 flu during the autopsy of an African-American soldier. Taubenberger's autopsy results showed that the soldier suffered a sickle-cell crisis that contributed to his death even though he had only one copy of the gene.[5] There have been calls to reclassify sickle cell trait as a disease state, based on its malignant clinical presentations.[6] Significance may be greater during exercise.[7]
In athletes
In some cases, athletes with sickle cell trait do not achieve the same level of performance as elite athletes with normal hemoglobin AA. Athletes with sickle cell trait and their instructors must be aware of the dangers of the condition during anaerobic exertion especially in hot and dehydrated conditions.[8] In rare cases, exercise-induced dehydration or exhaustion may cause healthy red blood cells to turn sickle-shaped, which can cause death during sporting activities.[9]
While more research is necessary on the topic, the correlation found between individuals with sickle cell trait and an increased risk of sudden death appears to be related to microcirculatory disorders, during exercise.[10] In recent years the NCAA has partnered with the ACSM and issued a joint statement, warning athletes about both the prevalence and the potential risk factors of sickle cell trait.[11] The NCAA has also recently encouraged athletes to become aware of their sickle cell trait status, as the trait itself does not typically result in symptoms under normal conditions but can become dangerous during extreme physical activity similar to the daily training that athletes undergo. Normal hemoglobin (and hemoglobin S in the presence of oxygen) contains a deformability characteristic that allows erythrocytes to essentially squeeze their way into smaller vessels, including those involved in microcirculation to the capillaries within muscle tissue as well as blood supply embedded within organ tissues. When hemoglobin S is deprived of oxygen, it can polymerize, which is what is proposed to cause the "sickled" cells.[10] The sickled erythrocytes present a decreased deformability when compared to normal erythrocytes, leading to distress in circulation into the smaller vessels involved in microcirculation, particularly, in this case, the capillaries embedded in muscle tissue.
The resulting microvasculatory distress in capillaries specific to muscle tissue can cause acute rhabdomyolysis and necrosis within the muscle cells.[11][12] The inflammation and leakage of intracellular material resulting from muscle cell necrosis releases a particular protein, myoglobin, into the blood stream. While necessary in muscle tissue to bind iron and oxygen, myoglobin circulating through the bloodstream can break down into smaller compounds that damage kidney cells, leading to various complications, such as those seen in sickle cell trait athletes during high levels of physical exertion.[13]
Because of the link between deformability and sickled cells, deformability can be used to evaluate the amount of sickled cells in the blood. Deformability of the erythrocytes that cause the microcirculatory distress can be demonstrated through various other hemorheological characteristics.[10] In order to determine the deformability of erythrocytes multiple factors including blood and plasma viscosity and hematocrit (a calculation of the percent of red blood cells present in the blood) are measured.[8][10]
Alpha-thalassemia
Alpha-thalassemia, like sickle cell trait, is typically inherited in areas with increased exposure to malaria. It manifests itself as a decreased expression of alpha-globin chains, causing an imbalance and excess of beta-globin chains, and can occasionally result in anemic symptoms. The abnormal hemoglobin can cause the body to destroy red blood cells, essentially causing anemia.[14]
In endurance-trained individuals with sickle cell trait the presence of alpha-thalassemia has been shown to act protectively against microvasculatory distress before, during, and after exercise.[10]
Signs, symptoms, and prevention
Because of the microcirculatory distress, a telltale sign or symptom of a potential sickling collapse is cramping. Specifically to sickle cell trait, cramping occurs in the lower extremities and back in athletes undergoing intense physical activity or exertion.[12] In comparison to heat cramps, sickling cramps are less intense in terms of pain and have a weakness and fatigue associated with them, as opposed to tightly contracted muscles that lock up during heat cramps.
A sickling collapse comes on slowly, following cramps, weakness, general body aches and fatigue.[12][13] Individuals with known positive sickle cell trait status experiencing significant muscle weakness or fatigue during exercise should take extra time to recover and hydrate before returning to activity in order to prevent further symptoms.[15]
A collapse can be prevented by taking steps to ensure sufficient oxygen levels in the blood. Among these preventative measures are proper hydration[8] and gradual acclimation to conditions such as heat, humidity, and decreased air pressure due to higher altitude.[11][12][15] Gradual progression of exertion levels also helps athletes’ bodies adjust and compensate, gaining fitness slowly over the course of several weeks.[11][12][16]
Association with malaria
Sickle cell trait provides a survival advantage over people with normal hemoglobin in regions where malaria is endemic. The trait is known to cause significantly fewer deaths due to malaria, especially when Plasmodium falciparum is the causative organism. This is a prime example of natural selection, evident by the fact that the geographical distribution of the gene (for hemoglobin S) and the distribution of malaria in Africa virtually overlap. Because of the unique survival advantage, people with the trait become increasingly numerous as the number of malaria-infected people increases. Conversely, people who have normal hemoglobin tend to succumb to the complications of malaria.
Although the precise mechanism for this phenomenon is not known, a several factors are believed to be responsible.
- Infected erythrocytes (Red Blood cells) tend to have lower oxygen tension, because it is significantly reduced by the parasite. This causes sickling of that particular erythrocyte, signalling the phagocytes to get rid of the cell and hence the parasite within.
- Since the sickling of parasite infected cells is higher, these selectively get removed by the reticulo-endothelial system, thus sparing the normal erythrocytes.
- Excessive vacuole formation occurs in those parasites infecting sickle cells.
- Sickle trait erythrocytes produce higher levels of the superoxide anion and hydrogen peroxide than do normal erythrocytes, both are toxic to malarial parasites.[17]
The sickle cell trait was found to be 50% protective against mild clinical malaria, 75% protective against admission to the hospital for malaria, and almost 90% protective against severe or complicated malaria.[18]
Established associations
- hematuria[19]
- hyposthenuria[20]
- renal medullary carcinoma, a cancer affecting the kidney, is a very rare complication seen in patients with sickle cell trait.[21]
- renal papillary necrosis[19] (only considered "possible" by some sources)[22]
- splenic infarcts at high altitude.[23] Surgery may not always be necessary.[24]
- Sudden deaths during physical exertion in African-American US army recruits[25][26]
- urinary tract infection[27]
Suggested
- Probable:[28] complicated hyphema, venous thromboembolic events, fetal loss, neonatal deaths, and preeclampsia
- Possible:[28] acute chest syndrome, asymptomatic bacteriuria, and anemia in pregnancy
- Insufficient evidence:[28] retinopathy, cholelithiasis, priapism,[29] leg ulcers, liver necrosis, avascular necrosis of the femoral head, and stroke. An association with complicated migraine headaches has been suggested.[30]
There have been reports of pulmonary venous thromboembolism in pregnant women with sickle cell trait,[31] or men during prolonged airflight, mild strokes and abnormalities on PET scans in children with the trait
Sickle cell trait appears to worsen the complications seen in diabetes mellitus type 2 (retinopathy, nephropathy and proteinuria)[32] and provoke hyperosmolar diabetic coma nephropathy especially in male patients.
See also
References
- ↑ http://www.ncbi.nlm.nih.gov/books/NBK21226[]
- ↑ Okpala, Iheanyi (2008). Practical Management of Haemoglobinopathies. John Wiley & Sons. p. 21. ISBN 1405140208. Retrieved 2 June 2016.
- ↑ Ragusa, A.; Frontini, V.; Lombardo, M.; Amata, S.; Lombardo, T.; Labie, D.; Krishnamoorthy, R.; Nagel, R. L. (1992). "Presence of an African β-globin gene cluster haplotype in normal chromosomes in sicily". American Journal of Hematology. 40 (4): 313–5. doi:10.1002/ajh.2830400413. PMID 1503087.
- ↑ Roach, E. S. (2005). "Sickle Cell Trait". Archives of Neurology. 62 (11): 1781–2. doi:10.1001/archneur.62.11.1781. PMID 16286558.
- ↑ "From 1918 Autopsy, A First Glimpse of Sickle Cell — and a Warning" www.wired.com
- ↑ Ajayi, A.A. Leslie (2005). "Should the sickle cell trait be reclassified as a disease state?". European Journal of Internal Medicine. 16 (6): 463. doi:10.1016/j.ejim.2005.02.010. PMID 16198915.
- ↑ Connes, Philippe; Reid, Harvey; Hardy-Dessources, Marie-Dominique; Morrison, Errol; Hue, Olivier (2008). "Physiological Responses of Sickle Cell Trait Carriers during Exercise". Sports Medicine. 38 (11): 931–46. doi:10.2165/00007256-200838110-00004. PMID 18937523.
- 1 2 3 Tripette, J.; Loko, G.; Samb, A.; Gogh, B. D.; Sewade, E.; Seck, D.; Hue, O.; Romana, M.; Diop, S.; Diaw, M.; Brudey, K.; Bogui, P.; Cisse, F.; Hardy-Dessources, M.-D.; Connes, P. (2010). "Effects of hydration and dehydration on blood rheology in sickle cell trait carriers during exercise". AJP: Heart and Circulatory Physiology. 299 (3): H908–14. doi:10.1152/ajpheart.00298.2010. PMID 20581085.
- ↑ Eichner, ER (2007). "Sickle cell trait". Journal of Sport Rehabilitation. 16 (3): 197–203. PMID 17923725.
- 1 2 3 4 5 Monchanin, Geraldine; Connes, Philippe; Wouassi, Dieudonne; Francina, Alain; Djoda, Bernard; Banga, Pierre Edmond; Owona, Francois Xavier; Thiriet, Patrice; Massarelli, Raphael; Martin, Cyril (2005). "Hemorheology, Sickle Cell Trait, and α-Thalassemia in Athletes: Effects of Exercise". Medicine and Science in Sports and Exercise. 37 (7): 1086–92. PMID 16015123.
- 1 2 3 4 http://www.ncaa.org/health-and-safety/medical-conditions/acsm-and-ncaa-joint-statement-sickle-cell-trait-and-exercise
- 1 2 3 4 5 http://www.nata.org/sites/default/files/SickleCellTraitAndTheAthlete.pdf[]
- 1 2 MedlinePlus Encyclopedia Rhabdomyolysis
- ↑ http://www.hematology.org/About/History/50-Years/1534.aspx
- 1 2 http://www.sicklecelldisease.org/index.cfm?page=sickle-cell-trait-athletics[]
- ↑ "Sickle Cell Trait". MetroHealth. Retrieved January 31, 2016.
- ↑ "Malaria and the Sickle hemoglobin gene". Brigham and Women's Hospital (BWH).
- ↑ Williams, Thomas N.; Mwangi, Tabitha W.; Wambua, Sammy; Alexander, Neal D.; Kortok, Moses; Snow, Robert W.; Marsh, Kevin (2005). "Sickle Cell Trait and the Risk ofPlasmodium falciparumMalaria and Other Childhood Diseases". The Journal of Infectious Diseases. 192 (1): 178–86. doi:10.1086/430744. PMC 3545189
 . PMID 15942909.
. PMID 15942909. - 1 2 Zadeii, Gino; Lohr James W. (1997). "Renal Papillary Necrosis in a Patient with Sickle Cell Trait". Journal of the American Society of Nephrology. 8 (6): 1034–9. PMID 9189873.
- ↑ Gupta AK, Kirchner KA, Nicholson R, et al. (December 1991). "Effects of alpha-thalassemia and sickle polymerization tendency on the urine-concentrating defect of individuals with sickle cell trait". J. Clin. Invest. 88 (6): 1963–8. doi:10.1172/JCI115521. PMC 295777
 . PMID 1752955.
. PMID 1752955. - ↑ Davis, Charles J.; Mostofi, F. K.; Sesterhenn, Isabell A. (1995). "Renal Medullary Carcinoma The Seventh Sickle Cell Nephropathy". The American Journal of Surgical Pathology. 19 (1): 1–11. doi:10.1097/00000478-199501000-00001. PMID 7528470.
- ↑ Mary Louise Turgeon (2005). Clinical hematology: theory and procedures. Lippincott Williams & Wilkins. pp. 179–. ISBN 978-0-7817-5007-3. Retrieved 6 May 2010.
- ↑ Amit K. Ghosh (13 June 2008). Mayo Clinic Internal Medicine Review: Eighth Edition. Informa Health Care. pp. 425–. ISBN 978-1-4200-8478-8. Retrieved 6 May 2010.
- ↑ Sheikha Anwar (2005). "Splenic syndrome in patients at high altitude with unrecognized sickle cell trait: splenectomy is often unnecessary". Canadian Journal of Surgery. 48 (5): 377–81. PMC 3211898
 . PMID 16248136.
. PMID 16248136. - ↑ Kark, John A.; Posey, David M.; Schumacher, Harold R.; Ruehle, Charles J. (1987). "Sickle-Cell Trait as a Risk Factor for Sudden Death in Physical Training". New England Journal of Medicine. 317 (13): 781–7. doi:10.1056/NEJM198709243171301. PMID 3627196.
- ↑ Mitchell, Bruce L. (2007). "Sickle Cell Trait and Sudden Death—Bringing it Home". Journal of the National Medical Association. 99 (3): 300–5. PMC 2569637
 . PMID 17393956.
. PMID 17393956. - ↑ Betty Pace (2007). Renaissance of Sickle Cell Disease Research in the Genome Era. Imperial College Press. pp. 62–. ISBN 978-1-86094-645-5. Retrieved 6 May 2010.
- 1 2 3 Tsaras G, Owusu-Ansah A, Boateng FO, Amoateng-Adjepong Y (June 2009). "Complications associated with sickle cell trait: a brief narrative review". Am. J. Med. 122 (6): 507–12. doi:10.1016/j.amjmed.2008.12.020. PMID 19393983.
- ↑ Birnbaum BF, Pinzone JJ (2008). "Sickle cell trait and priapism: a case report and review of the literature". Cases J. 1: 429. doi:10.1186/1757-1626-1-429. PMC 2628646
 . PMID 19116025.
. PMID 19116025. - ↑ Osuntokun, B. O.; Osuntokun, O. (1972). "Complicated Migraine and Haemoglobin AS in Nigerians". BMJ. 2 (5814): 621–2. doi:10.1136/bmj.2.5814.621. PMC 1788370
 . PMID 5031686.
. PMID 5031686. - ↑ Austin H, Key NS, Benson JM, et al. (August 2007). "Sickle cell trait and the risk of venous thromboembolism among blacks" (Free full text). Blood. 110 (3): 908–12. doi:10.1182/blood-2006-11-057604. ISSN 0006-4971. PMID 17409269.
- ↑ Ajayi AA, Kolawole BA (August 2004). "Sickle cell trait and gender influence type 2 diabetic complications in African patients". Eur. J. Intern. Med. 15 (5): 312–315. doi:10.1016/j.ejim.2004.06.003. ISSN 0953-6205. PMID 15450989.