Vagal tone
Vagal tone is an internal biological process referring to the activity of the vagus nerve (the tenth cranial nerve), which originates in the medulla oblongata of the brainstem. The vagus nerve serves as the key component of the parasympathetic branch of the autonomic nervous system, which homeostatically regulates the resting state of the majority of the body's internal organ systems that operate on a largely subconscious level, such as the heart, lungs, eyes, glands and digestive tract.[1] Due to the regulatory nature of the parasympathetic nervous system (PSNS), vagal activity is continuous, chronic, and passive ("tone" in this usage is analogous to "tension",[2] reflecting a sense of continuous baseline activity, much like muscle tone relies on nervous baseline activity).
In the context of psychophysiological research, vagal tone (and specifically its influence on heart rate) represents an index for the functional state of the entire parasympathetic nervous system. Heart rate is normally controlled by multiple centers in the brainstem; one of these centers, the nucleus ambiguus, increases parasympathetic nervous system input to the heart via the vagus nerve. Vagal tone decreases heart rate by inhibiting the firing rate of the sinoatrial node (S-A node, the usual natural pacemaker tissue of the heart). The absolute level of cardiac vagal activity or vagal tone appears to result from the excitatory drive from peripheral baroreceptors. In animals, cardiac vagal activity disappears at very low pressures or if the afferent nerves are cut.[3] Thus, a major determinant of resting heart rate is the beat to beat activation of the arterial baroreflex with each cardiac cycle. Cardiac vagal tone has been treated as a physiologic substrate of regulation of emotion and arousal.[4]
Relation to respiratory sinus arrhythmia
Respiratory sinus arrhythmia (RSA) is a naturally occurring variation in heart rate that occurs during a breathing cycle. RSA is also a measure of parasympathetic nervous system activity – which denotes "rest and digest" behaviors.
Vagal tone cannot be directly measured. Instead, other biological processes are measured that represent the functionality of vagal tone. An increase in vagal tone both slows the heart and makes heart rate more variable (i.e. there is more beat-to-beat change between heart beats). During the process of RSA inhalation temporarily suppresses vagal activity, causing an immediate increase in heart rate. Exhalation then decreases heart rate as it causes vagal activity to resume. Thus, while vagal tone is not explicitly measured, the resultant changes in heart rate are. This is done by measuring periodic changes in the heart rate during a resting state of cardiovascular activity, a process known as heart rate variability (HRV). There are about 40 published methods of quantifying HRV, but the vast majority of studies use only a few of the available measurements. Most common is high-frequency HRV, a measurement of the amount of heart rate variability there is between typical breathing cycles (approximately 2.5 to 6.7 seconds).
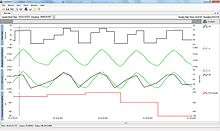
On an electrocardiogram ECG, RSA is seen as subtle changes in the R-R interval (time between two of the distinctive, large, upward "R" spikes on an electrocardiogram) synchronized with respiration. The R-R interval on an ECG is shortened during inhalation and prolonged during expiration. Meditation and relaxed breathing techniques can temporarily alter RSA.[5]
Age differences
RSA is very pronounced in children, but without sufficient cardiovascular exercise it gradually disappears as a person approaches his/her teenage years. Typically, expression of RSA decreases with age; however, adults in excellent cardiovascular health, such as endurance runners, swimmers, and cyclists, are likely to have a more pronounced RSA. Professional athletes typically maintain very high vagal tone and RSA levels. RSA also becomes less prominent in individuals with diabetes and cardiovascular disease.[6]
Biological findings
Studies have shown that the efficiency of pulmonary gas exchange is improved by RSA, suggesting that RSA may play an active physiological role. The matched timing of alveolar ventilation and its perfusion with RSA within each respiratory cycle could save energy expenditure by suppressing unnecessary heartbeats during expiration and ineffective ventilation during the ebb of perfusion (delivery of blood from arteries to capillaries for oxygenation and nutrition).[7][8]
RSA or heart rate variability in synchrony with respiration is a biological phenomenon, which may have a positive influence on gas exchange at the level of the lung via efficient ventilation/perfusion matching.[9]
Historically, respiratory sinus arrhythmia was believed to be pathological, and extended bed rest was traditionally prescribed until work by Sir James Mackenzie disproved this idea.[10]
Psychological findings
Due to age differences in expression of RSA, the majority of vagal tone research as it relates to social behavior and human psychology has focused on children. Typically, researchers are concerned with baseline vagal tone, treating it either as a potential predictor of behavior or examining its relationship with mental health (particularly emotion regulation, MDD, anxiety, and internalizing and externalizing disorders).[11][12]
Research indicates that children with more secure attachments with their mothers exhibited greater empathetic responsiveness, less social inhibition, and higher vagal tone, again highlighting the vagus nerve's regulatory effect on emotional and social function.[4]
References
- ↑ Porges SW, Doussard-Roosevelt JA, Maiti AK (1994). "Vagal tone and the physiological regulation of emotion". Monographs of the Society for Research in Child Development. 59: 167–186. doi:10.1111/j.1540-5834.1994.tb01283.x. JSTOR 1166144.
- ↑ Heathers, J. (2006). "Introduction to vagal tone".
- ↑ Kunze, D.L. (1972). "Reflex discharge patterns of cardiac vagal efferent fibres". Journal of Physiology. 222 (1): 1–15. PMC 1331413
 . PMID 4338691.
. PMID 4338691. - 1 2 Diamond LM, Fagundes CP, Butterworth MR (2012). "Attachment style, vagal tone, and empathy during mother–adolescent interactions". Journal of Research on Adolescence. 22 (1): 165–184. doi:10.1111/j.1532-7795.2011.00762.x.
- ↑ Peng CK, Henry IC, Mietus JE, Hausdorff JM, Khalsa G, Benson H, Goldberger AL (2004). "Heart rate dynamics during three forms of meditation" (PDF). International Journal of Cardiology. 95 (1): 19–27. doi:10.1016/j.ijcard.2003.02.006. PMID 15159033.
- ↑ "Respiratory sinus arrhythmia and diseases of aging: Obesity, diabetes mellitus, and hypertension". Biological Psychology. 74: 212–223. doi:10.1016/j.biopsycho.2006.07.006. Retrieved 2014-11-06.
- ↑ Ben-Tal, A; Shamailov, SS; Paton, JFR (2012). "Evaluating the physiological significance of respiratory sinus arrhythmia: looking beyond ventilation-perfusion efficiency". J Physiol. 590 (8): 1989–2008. doi:10.1113/jphysiol.2011.222422.
- ↑ Hayano, J (1996). "Respiratory sinus arrhythmia. A phenomenon improving pulmonary gas exchange and circulatory efficiency". Circulation. 94 (4): 842–7. doi:10.1161/01.cir.94.4.842.
- ↑ Yasuma F, et al. (Feb 2004). "Respiratory sinus arrhythmia: why does the heartbeat synchronize with respiratory rhythm?". Chest. 125 (2): 683–90. doi:10.1378/chest.125.2.683. PMID 14769752.
- ↑ Moorhead R. (Jan 1999). "Sir James Mackenzie (1853-1925): views on general practice education and research". Journal of the Royal Society of Medicine. 92 (1): 38–43. PMC 1297041
 . PMID 10319040.
. PMID 10319040. - ↑ Connell, A.M.; Hughes-Scalise, A.; Klostermann, S.; Azem, T. (2011). "Maternal depression and the heart of parenting: Respiratory sinus arrhythmia and affective dynamics during parent–adolescent interactions". Journal of Family Psychology. 25 (5): 653–662. doi:10.1037/a0025225.
- ↑ Rottenberg, Jonathan; Clift, April; Bolden, Sarah; Saloman, Kristen (2007). "RSA fluctuation in major depressive disorder". Psychophysiology. 44: 450–458. doi:10.1111/j.1469-8986.2007.00509.x.
- Neff RA, Wang J, Baxi S, Evans C, Mendelowitz D (2003). "Respiratory sinus arrhythmia: endogenous activation of nicotinic receptors mediates respiratory modulation of brainstem cardioinhibitory parasympathetic neurons". Circ. Res. 93 (6): 565–72. doi:10.1161/01.RES.0000090361.45027.5B. PMID 12907666.