Phrenic nerve
| Phrenic nerve | |
|---|---|
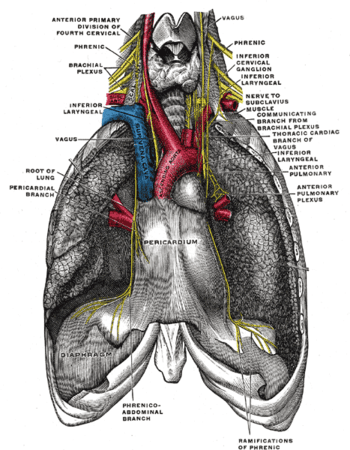 The phrenic nerve and its relations with the vagus nerve. (Phrenic labeled at upper left and right.) | |
 Plan of the cervical plexus. (Phrenic labeled at bottom right.) | |
| Details | |
| From | C3-c5 of cervical plexus |
| Innervates | Diaphragm |
| Identifiers | |
| Latin | nervus phrenicus |
| TA | A14.2.02.028 |
| FMA | 6191 |
The phrenic nerve is a nerve that originates in the neck (C3-C5) and passes down between the lung and heart to reach the diaphragm. It is important for breathing, as it passes motor information to the diaphragm and receives sensory information from it. There are two phrenic nerves, a left and a right one.
The phrenic nerve originates mainly from the 4th cervical nerve, but also receives contributions from the 5th and 3rd cervical nerves (C3-C5) in humans.[1] Thus, the phrenic nerve receives innervation from parts of both the cervical plexus and the brachial plexus of nerves.
The phrenic nerves contain motor, sensory, and sympathetic nerve fibers. These nerves provide the only motor supply to the diaphragm as well as sensation to the central tendon. In the thorax, each phrenic nerve supplies the mediastinal pleura and pericardium.
Structure
The phrenic nerve descends obliquely with the internal jugular vein across the anterior scalene, deep to the prevertebral layer of deep cervical fascia and the transverse cervical and suprascapular arteries. On the left, the phrenic nerve crosses anterior to the first part of the subclavian artery. On the right, it lies on the anterior scalene muscle and crosses anterior to the 2nd part of the subclavian artery. On both sides, the phrenic nerve runs posterior to the subclavian vein as it enters the thorax where it runs anterior to the root of the lung and between the fibrous pericardium and mediastinal face of the parietal pleura.[1]
Found in the middle mediastinum, both phrenic nerves run from C3, C4, and C5 along the anterior scalene muscle deep to the carotid sheath.
- The right phrenic nerve passes over the brachiocephalic artery, posterior to the subclavian vein, and then crosses the root of the right lung anteriorly and then leaves the thorax by passing through the vena cava hiatus opening in the diaphragm at the level of T8. The right phrenic nerve passes over the right atrium.
- The left phrenic nerve passes over the pericardium of the left ventricle and pierces the diaphragm separately.
The pericardiacophrenic arteries and veins travel with their respective phrenic nerves.
The phrenic nerve can be marked by a line connecting these two points:
- 1st point can be labelled 3.5 cm at the level of the thyroid cartilage from the midsagittal plane.
- 2nd point is at the medial end of the clavicle.
Variation
The contribution of the 5th cervical nerve may stem from an accessory phrenic nerve. Phrenic nerve in its early course close to its origin, was giving a communicating branch to C5 root of brachial plexus. The phrenic nerve at the level of root of neck just before entering the thorax was placed in front of the subclavian vein. Usually it is placed posterior in between subclavian vein and artery.[2]
Most often it is a branch of the nerve to the subclavius and may contain numerous phrenic nerve fibers. If the accessory phrenic nerve is present, it lies lateral to the main nerve and descends posterior and occasionally inferior to the subclavian vein. The accessory phrenic nerve connects to the phrenic nerve in the thorax or the root of the neck.[1]
In canines the phrenic nerve arises from C5-C7 with occasional small contributions from C4.[3] In the cat, horse, ox, and small ruminant the phrenic nerve arises variably from C4-C7.
Function
Both of these nerves supply motor fibers to the diaphragm and sensory fibers to the fibrous pericardium, mediastinal pleura, and diaphragmatic peritoneum.
Some sources describe the right phrenic nerve as innervating the gallbladder, other sources make no such mention. [4]
Clinical significance

Pain arising from structures supplied by the phrenic nerve is often "referred" to other somatic regions served by spinal nerves C3-C5. For example, a subphrenic abscess beneath the right diaphragm might cause a patient to feel pain in the right shoulder.
Irritation of the phrenic nerve (or the tissues supplied by it) leads to the hiccup reflex. A hiccup is a spasmodic contraction of the diaphragm, which pulls air against the closed folds of the larynx.
The phrenic nerve must be identified during thoracic surgery and preserved. To confirm the identity of the phrenic nerve, gently manipulate it to elicit a dartle (diaphragmatic startle) response.[5] The right phrenic nerve may be crushed by the vena cava clamp during liver transplantation.[6] Severing the phrenic nerve, or a phrenectomy,[7] will paralyse that half of the diaphragm. Diaphragm paralysis is best demonstrated by sonography.[6] Breathing will be made more difficult but will continue provided the other nerve is intact.
The phrenic nerve arises from the neck (C3-C5) and innervates the diaphragm, which is much lower. Hence, patients suffering spinal cord injuries below the neck are still able to breathe effectively, despite any paralysis of the lower limbs.
Brachial plexus injuries can cause paralysis to various regions in the arm, forearm, and hand depending on the severed nerves. The resulting palsy has been clinically treated using the phrenic nerve as a donor for neurotization of the musculocutaneous nerve and the median nerve.[8] This treatment has a high success rate (84.6%) in partial to full restoration of the innervation to the damaged nerve.[8] Furthermore, this procedure has resulted in restored function to nerves in the brachial plexus with minimal impact to respiratory function of the phrenic nerve. The instances where pulmonary vital capacity is reduced have typically been a result of use of the right phrenic as the donor for the neurotization whereas use of left phrenic nerve has not been significantly linked to reduced pulmonary vital capacity.[9]
Additional images
 Transverse section of thorax, showing relations of pulmonary artery.
Transverse section of thorax, showing relations of pulmonary artery.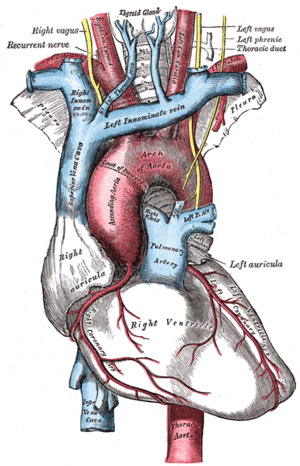 The arch of the aorta, and its branches.
The arch of the aorta, and its branches. Superficial dissection of the right side of the neck, showing the carotid and subclavian arteries.
Superficial dissection of the right side of the neck, showing the carotid and subclavian arteries. The right brachial plexus with its short branches, viewed from in front.
The right brachial plexus with its short branches, viewed from in front.
See also
References
- 1 2 3 Moore, Keith L. (1999). Clinically oriented anatomy. Philadelphia: Lippincott Williams & Wilkins. ISBN 0-683-06141-0.
- ↑ Prakash; Prabhu, L. V.; Madhyastha, S; Singh, G (2007). "A variation of the phrenic nerve: Case report and review" (PDF). Singapore Medical Journal. 48 (12): 1156–7. PMID 18043847.
- ↑ Evans, Howard (1979). Miller's Anatomy of the Dog. Philadelphia, PA: W. B. Saunders Company. p. 978. ISBN 0-7216-3438-9.
- ↑ Alexander, William (1940). "The innervation of the biliary system". Journal of Comparitive Neurology. 72 (2): 357–370. doi:10.1002/cne.900720205.
- ↑ Dalman, Ronald; Thompson, Robert (2015). "7. Neurogenic Thoracic Outlet Syndrome Exposure and Decompression: Supraclavicular". Operative Techniques in Vascular Surgery. Philadelphia, PA: Wolters Kluwer Health. p. 50. ISBN 9781451190205.
- 1 2 McAlister, Vivian C.; Grant, David R.; Roy, Andre; Brown, William F.; Hutton, Linda C.; Leasa, David J.; Ghent, Cameron N.; Veitch, James E.; Wall, William J. (1993). "Right phrenic nerve injury in orthotopic liver transplantation". Transplantation. 55 (4): 826–30. doi:10.1097/00007890-199304000-00027. PMID 8475559.
- ↑ Hine, Maynard Kiplinger (1975). Review of dentistry: questions and answers (6th ed.). Mosby. p. 421. ISBN 0-8016-2196-8.
- 1 2 Yu-Dong, G., Min-Ming, W., Yi-Lu, Z., Jia-Ao, Z., Gao-Meng, Z., De-Song, C., Ji-Geng, Y. and Xiao-Ming, C. (1989), Phrenic nerve transfer for brachial plexus motor neurotization. Microsurgery, 10: 287–289. doi: 10.1002/micr.1920100407
- ↑ Luedemann, Wolf, Michael Hamm, Ulrike Blömer, Madjid Samii, and Marcos Tatagiba. "Brachial Plexus Neurotization with Donor Phrenic Nerves and Its Effect on Pulmonary Function." Journal of Neurosurgery 96.3 (2002): 523-26. Web.
External links
- -1402273763 at GPnotebook
- Anatomy figure: 19:04-05 at Human Anatomy Online, SUNY Downstate Medical Center - "Left side of the mediastinum."
- Anatomy figure: 25:03-15 at Human Anatomy Online, SUNY Downstate Medical Center - "Diagram of the cervical plexus."