Organophosphate poisoning
| Organophosphate poisoning | |
|---|---|
| organophosphate toxicity, organophosphate overdose, organophosphate intoxication | |
 | |
| Specialty | emergency medicine |
| Symptoms | increased saliva, diarrhea, small pupils, muscle tremors, confusion |
| Usual onset | within 12 hours[1] |
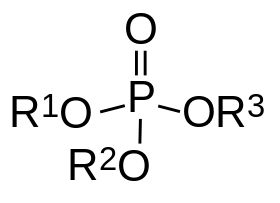
| Causes | organophosphates[2] |
| Diagnostic method | based on symptoms and confirmed by butyrylcholinesterase[2] |
| Differential diagnosis | carbamate poisoning[2] |
| Prevention | decreasing access[2] |
| Medication | atropine, oximes, diazepam[2] |
| Frequency | nearly 3 million per year[3] |
| Deaths | >200,000 per year[2] |
Organophosphate poisoning is poisoning due to organophosphates (OPs). Organophosphate are used as insecticides, medications, and nerve agents.[4] Symptoms include increased saliva and tear production, diarrhea, vomiting, small pupils, sweating, muscle tremors, and confusion.[2] While onset of symptoms is often rapid they can take up to 12 hours to appear.[1] Symptoms can last for days to weeks.[2]
Organophosphate poisoning occurs most commonly as a suicide attempt in farming areas of the developing world and less commonly by accident.[2] Exposure can be from drinking, breathing in the vapors, or skin exposure.[4] The underlying mechanism involves the inhibition of acetylcholinesterase (AChE), leading to the build up of acetylcholine (ACh) in the body. Diagnosis is typically based on the symptoms and can be confirmed by measuring butyrylcholinesterase activity in the blood. Carbamate poisoning can present similarly.[2]
Prevention includes banning very toxic types of organophosphates.[2] In those who have organophosphate poisoning the primary treatments are atropine, oximes such as pralidoxime, and diazepam.[2][4] General measures such as oxygen and intravenous fluids are also recommended. Attempts to decontaminate the stomach, with activated charcoal or other means, has not been shown to be useful. While there is a theoretical risk of health care workers taking care of a poisoned person becoming poisoned themselves, the degree of risk appears to be very small.[2]
OPs are one of the most common causes of poisoning worldwide.[2] There are nearly 3 million poisonings per year resulting in two hundred thousand death.[2][3] Around 15% of people who are poisoned die as a result.[2] Organophosphate poisoning has been reported at least since 1962.[5]
Signs and symptoms
The health effects associated with organophosphate poisoning are a result of excess acetylcholine (ACh) present at different nerves and receptors in the body because acetylcholinesterase is blocked. Accumulation of ACh at motor nerves causes overstimulation of nicotinic expression at the neuromuscular junction. When this occurs symptoms such as muscle weakness, fatigue, muscle cramps, fasciculation, and paralysis can be seen. When there is an accumulation of ACh at autonomic ganglia this causes overstimulation of nicotinic expression in the sympathetic system. Symptoms associated with this are hypertension, and hypoglycemia. Overstimulation of nicotinic acetylcholine receptors in the central nervous system, due to accumulation of ACh, results in anxiety, headache, convulsions, ataxia, depression of respiration and circulation, tremor, general weakness, and potentially coma. When there is expression of muscarinic overstimulation due to excess acetylcholine at muscarinic acetylcholine receptors symptoms of visual disturbances, tightness in chest, wheezing due to bronchoconstriction, increased bronchial secretions, increased salivation, lacrimation, sweating, peristalsis, and urination can occur.[6][7]
The effects of organophosphate poisoning on muscarinic receptors are recalled using the mnemonic SLUDGEM (salivation, lacrimation, urination, defecation, gastrointestinal motility, emesis, miosis)[8] An additional mnemonic is MUDDLES: miosis, urination, diarrhea, diaphoresis, lacrimation, excitation, and salivation.[9]
The onset and severity of symptoms, whether acute or chronic, depends upon the specific chemical, the route of exposure (skin, lungs, or GI tract), the dose, and the individuals ability to degrade the compound, which the PON1 enzyme level will affect.
Reproductive effects
Certain reproductive effects in fertility, growth, and development for males and females have been linked specifically to OP pesticide exposure. Most of the research on reproductive effects has been conducted on farmers working with pesticides and insecticdes in rural areas. For those males exposed to OP pesticides, poor semen and sperm quality have been seen, including reduced seminal volume and percentage motility, as well as a decrease in sperm count per ejacuate. In females menstrual cycle disturbances, longer pregnancies, spontaneous abortions, stillbirths, and some developmental effects in offspring have been linked to OP pesticide exposure. Prenatal exposure has been linked to impaired fetal growth and development. The effects of OP exposure on infants and children are at this time currently being researched to come to a conclusive finding.[10][11] Evidence of OP exposure in pregnant mothers are linked to several health effects in the fetus. Some of these effects include delayed mental development, Pervasive developmental disorder (PDD),[7] morphological abnormalities in the cerebral surface.[12] Studies observing prenatal exposure to OP pesticides used Latina women living in various agricultural communities in California as their focus. In these studies, exposure to OP pesticides were mainly measured in three ways : (1) using dialkyl phosphate (DAP) metabolites collected from urine (2) using pesticide-specific metabolites found in urine and (3) measuring cholinesterase (ChE) and butyryl cholinesterase (BChE).[13] It was found that high exposure to OP pesticides prenatally (measured by DAP in urine) is associated with lowered IQ scores in 7-year-old children. Higher DAP levels were associated with lower scores on four cognitive areas, with the strongest association in verbal comprehension.[14] A separate study also showed that higher prenatal chlorpyrifos (CPF) exposure was also linked to several brain anomalies. This studies used MRI and compared 20 low CPF exposure children to 20 high CPF exposure children. It was found that although overall brain size did not differ between exposure groups, there were significant areas of the brain that were enlarged in children with high exposure. These enlargements were primarily due to an increase of underlying white matter in the high exposure group. Enlargements were seen bilaterally in the superior temporal, posterior middle temporal, and inferior postcentral gyri, and superior frontal gyrus, straight gyrus, cuneus, and precuneus in the medial views of the right hemisphere.[15]
Neurotoxic effects
Neurotoxic effects have also been linked to poisoning with OP pesticides causing four neurotoxic effects in humans: cholinergic syndrome, intermediate syndrome, organophosphate-induced delayed polyneuropathy (OPIDP), and chronic organophosphate-induced neuropsychiatric disorder (COPIND). These syndromes result after acute and chronic exposure to OP pesticides.
Cholinergic syndrome occurs in acute poisonings with OP pesticides and is directly related to levels of AChE activity. Symptoms include miosis, sweating, lacrimation, gastrointestinal symptoms, respiratory difficulties, shortness of breath, slowed heart rate, cyanosis, vomiting, diarrhea, as well as other symptoms. Along with these central effects can be seen and finally seizures, convulsions, coma, respiratory failure. If the person survives the first day of poisoning personality changes can occur, aggressive events, psychotic episodes, disturbances and deficits in memory and attention, as well as other delayed effects. When death occurs, it is most commonly due to respiratory failure from the combination of central and peripheral effects, paralysis of respiratory muscles and depression of the brain respiratory center. For people afflicted with cholinergic syndrome, atropine sulfate combined with an oxime is used to combat the effects of the acute OP poisoning. Diazepam is sometimes also administered in combination with the atropine and oximes.[16]
The intermediate syndrome (IMS) appears in the interval between the end of the cholinergic crisis and the onset of OPIDP. Symptoms associated with IMS manifest within 24–96 hours after exposure. The exact etiology, incidence, and risk factors associated with IMS are not clearly understood, but IMS is recognized as a disorder of neuromuscular junctions. IMS occurs when a person has a prolonged and severe inhibition of AChE and has been linked to specific OP pesticides such as methylparathion, dichlorvos, and parathion. Patients present with increasing weakness of facial, neck flexor and respiratory muscles.
OPIDP occurs in a small percentage of cases, roughly two weeks after exposure, where temporary paralysis occurs. This loss of function and ataxia of peripheral nerves and spinal cord is the phenomenon of OPIDP. Once the symptoms begin with shooting pains in both legs, the symptoms continue to worsen for 3–6 months. In the most severe cases quadriplegia has been observed. Treatment only affects sensory nerves, not motor neurons which may permanently lose function. The aging and phosphorylation of more than 70% of functional NTE in peripheral nerves is one of the processes involved in OPIDP.[9][16] Standard treatments for OP poisoning are ineffective for OPIDP.
COPIND occurs without cholinergic symptoms and is not dependent on AChE inhibition. COPIND appears with a delay and is long lasting. Symptoms associated with COPIND include cognitive deficit, mood change, autonomic dysfunction, peripheral neuropathy, and extrapyramidal symptoms. The underlying mechanisms of COPIND have not been determined, but it is hypothesized that withdrawal of OP pesticides after chronic exposure or acute exposure could be a factor.[16]
Organophosphate pesticides are one of the top causes of poisoning worldwide, with an annual incidence of poisonings among agricultural workers varying from 3-10% per country[17]
Effects on developing animals
Evidence of exposure to OP pesticides during gestation and early postnatal period have been linked to neurodevelopmental effects in animals, specifically rats. Animals exposed in utero to chlorpyrifos exhibited decreased balance, poorer cliff avoidance, decreased locomotion, delays in maze performance, and increased gait abnormalities. Early gestation is believed to be a critical time period for the neurodevelopmental effects of pesticides. OP's affect the cholinergic system of fetuses, so exposure to chlorpyrifos during critical periods of brain development potentially could cause cellular, synaptic, and neurobehavioral abnormalities in animals.[14] In rats exposed to methyl parathion, studies found reduced AChE activity in all brain regions and subtle alterations in behaviors such as locomotor activity and impaired cage emergence. Organophosphates as whole have been linked to decreases in the length of limbs, head circumference, and slower rates of postnatal weight gain in mice.[7]
Cause
OP pesticide exposure occurs through inhalation, ingestion and dermal contact.[18] Because OP pesticides disintegrate quickly in air and light, they have been considered relatively safe to consumers.[19] However, OP residues linger on fruits and vegetables.[20] Certain OP pesticides have been banned for use on some crops, for example methyl parathion is banned from use on some crops while permitted on others.[21] The Environmental Working Group has developed lists for concerned consumers, identifying crops with the highest pesticide residue quantities and the lowest. The "Dirty Dozen" crops are updated yearly and in 2012 included apples, celery, sweet bell peppers, peaches, strawberries, imported nectarines, grapes, spinach, lettuce, cucumbers, domestic blueberries and potatoes.[22] Forty-five fruits and vegetables are listed by the Environmental Working Group as being regularly found with pesticide residue associated with OPs.
Examples
- Insecticides including malathion, parathion, diazinon, fenthion, dichlorvos, chlorpyrifos, ethion, trichlorfon
- Nerve gases including soman, sarin, tabun, VX
- Herbicides including tribufos [DEF], merphos are tricresyl phosphate–containing industrial chemicals.
Exposure to any one of the above-listed organophosphates occurs on a daily basis through inhalation, absorption, and ingestion, most commonly of food that has been treated with an organophosphate herbicide or insecticide. Exposure to these chemicals can occur at public buildings, schools, residential areas, and in agricultural areas. The chemicals chlorpyrifos and malathion have been linked to reproductive effects, neurotoxicity, kidney/liver damage, and birth defects. Dichlorvos has also been linked to reproductive effects, neurotoxicity, and kidney/liver damage, as well as being a possible carcinogen.[23]
Pathophysiology
Organophosphates inhibit AChE, causing OP poisoning by phosphorylating the serine hydroxyl residue on AChE, which inactivates AChE. AChE is critical for nerve function, so the irreversible blockage of this enzyme, which causes acetylcholine accumulation, results in muscle overstimulation. This causes disturbances across the cholinergic synapses and can only be reactivated very slowly, if at all. Paraoxonase (PON1) is a key enzyme involved in OP pesticides and has been found to be critical in determining an organism's sensitivity to OP exposure.
PON1 can inactivate some OPs through hydrolysis. PON1 hydrolyzes the active metabolites in several OP insecticides such as chlorpyrifos oxon, and diazoxon, as well as, nerve agents such as soman, sarin, and VX. PON1 hydrolyzes the metabolites, not the parent compounds of insectides.[24] The presence of PON1 polymorphisms causes there to be different enzyme levels and catalytic efficiency of this esterase, which in turn suggests that different individuals may be more susceptible to the toxic effect of OP exposure. The level of PON1 plasma hydrolytic activity provides more protection against OP pesticides. Rats injected with purified PON1 from rabbit serum were more resistant to acute cholinergic activity than the control rats. PON1 knockouts in mice are found to be more sensitive to the toxicity of pesticides, like chlorpyrifos. Animal experiments indicate that while PON1 plays a significant role in regulating the toxicity of OPs its degree of protection given depends on the compound (i.e. Chlorpyrifos oxon or diazoxon). The catalytic efficiency with which PON1 can degrade toxic OPs determines the degree of protection that PON1 can provide for organism. The higher the concentration of PON1 the better the protection provided. PON1 activity is much lower in neonates, so neonates are more sensitive to OP exposure.[24] In 2006, reports up to a 13-fold variation was seen in PON1 levels in adults, as well as, specifically regarding sensitivity to diazoxon, a variation up to 26 and 14-fold was reported in a group of newborns and Latino mothers. This wide range in variability of enzyme levels determining a humans sensitivity to various OPs is being researched further.[25]
Diagnosis
A number of measurements exist to assess exposure and early biological effects for organophosphate poisoning. Measurements of OP metabolites in both the blood and urine can be used to determine if a person has been exposed to organophosphates. Specifically in the blood, metabolites of cholinesterases, such as butyrylcholinesterase (BuChE) activity in plasma, neuropathy target esterase (NTE) in lymphocytes, and of acetylcholinesterase (AChE) activity in red blood cells.[24] Due to both AChE and BuChE being the main targets of organophosphates, their measurement is widely used as an indication of an exposure to an OP. The main restriction on this type of diagnosis is that depending on the OP the degree to which either AChE or BuChE are inhibited differs; therefore, measure of metabolites in blood and urine do not specify for a certain OP.[24][26] However, for fast initial screening, determining AChE and BuChE activity in the blood are the most widely used procedures for confirming a diagnosis of OP poisoning.[26] The most widely used portable testing device is the Test-mate ChE field test,[27][28]:13 which can be used to determine levels of Red Blood Cells (RBC), AChE and plasma (pseudo) cholinesterase (PChE) in the blood in about four minutes. This test has been shown to be just as effective as a regular laboratory test and because of this, the portable ChE field test is frequently used by people who work with pesticides on a daily basis.[29]
Treatment
Current antidotes for OP poisoning consist of a pretreatment with carbamates to protect AChE from inhibition by OP compounds and post-exposure treatments with anti-cholinergic drugs. Anti-cholinergic drugs work to counteract the effects of excess acetylcholine and reactivate AChE. Atropine can be used as an antidote in conjunction with pralidoxime or other pyridinium oximes (such as trimedoxime or obidoxime),[30][31] though the use of "-oximes" has been found to be of no benefit, or possibly harmful, in at least two meta-analyses.[32][33] Atropine is a muscarinic antagonist, and thus blocks the action of acetylcholine peripherally.[34] These antidotes are effective at preventing lethality from OP poisoning, but current treatment lack the ability to prevent post-exposure incapacitation, performance deficits, or permanent brain damage.[35] While the efficacy of atropine has been well-established, clinical experience with pralidoxime has led to widespread doubt about its efficacy in treatment of OP poisoning.[36]
Enzyme bioscavengers are being developed as a pretreatment to sequester highly toxic OPs before they can reach their physiological targets and prevent the toxic effects from occurring. Significant advances with cholinesterases (ChEs), specifically human serum BChE (HuBChE) have been made. HuBChe can offer a broad range of protection for nerve agents including soman, sarin, tabun, and VX. HuBChE also possess a very long retention time in the human circulation system and because it is from a human source it will not produce any antagonistic immunological responses. HuBChE is currently being assessed for inclusion into the protective regimen against OP nerve agent poisoning.[35] Currently there is potential for PON1 to be used to treat sarin exposure, but recombinant PON1 variants would need to first be generated to increase its catalytic efficiency.
One other agent that is being researched is the Class III anti-arrhythmic agents. Hyperkalemia of the tissue is one of the symptoms associated with OP poisoning. While the cellular processes leading to cardiac toxicity are not well understood, the potassium current channels are believed to be involved. Class III anti-arrhythmic agents block the potassium membrane currents in cardiac cells, which makes them a candidate for become a therapeutic of OP poisoning.[37]
History
Ginger Jake
A striking example of OPIDN occurred during the 1930s Prohibition Era when thousands of men in the American South and Midwest developed arm and leg weakness and pain after drinking a "medicinal" alcohol substitute. The drink, called "Ginger Jake," contained an adulterated Jamaican ginger extract containing tri-ortho-cresyl phosphate (TOCP) which resulted in partially reversible neurologic damage. The damage resulted in the limping "Jake Leg" or "Jake Walk" which were terms frequently used in the blues music of the period. Europe and Morocco both experienced outbreaks of TOCP poisoning from contaminated abortifacients and cooking oil, respectively.[38][39]
Gulf War syndrome
Research has linked the neurological abnormalities found in Persian Gulf War veterans who suffer from Gulf War syndrome to exposure to wartime combinations of organophosphate chemical nerve agents. Before, it was believed that veterans were suffering from a psychologically based disorder or depression, most likely post-traumatic stress disorder (PTSD). Many veterans were given pyridostigmine bromide (PB) pills to protect against nerve gas agents such as sarin and soman. During the war veterans were exposed to combinations of organophosphate nerve agents, which produced symptoms associated with chronic organophosphate-induced delayed polyneuropathy (OPIDP) syndrome. Similar symptoms found in the veterans were the same symptoms reported for individuals in occupational settings who were acutely poisoned by organophosphates, such as chlorpyrifos. Studies found veterans experienced deficits in intellectual and academic abilities, simple motor skills, memory impairment, and impaired emotional function. These symptoms indicate brain damage, not a psychologically based disorder.[40][41][42]
Society and culture
British Government
Recent press stories reveal a deliberate coverup and lying by the UK government.[43]
United States
Under a 1988 amendment to the Federal Insecticide, Fungicide and Rodenticide Act (FIFRA), the U.S. Environmental Protection Agency (EPA) regulates organophosphate pesticides[44] Its focus was initially on registering pesticides for use on food crops. No pesticide can be sold in the United States before the EPA has reviewed the manufacture's application for registration and determined that the use of the product will not present an unreasonable risk to the public or the environment.[45] In 1996, with the passage of the Food Quality Protection Act, Congress required the EPA to reassess all existing pesticide tolerances with specific consideration for children.[46] This resulted in a 10-year review process of the health and environmental effects of all pesticides, beginning with the organophosphates. As part of that process, in 1999 the EPA announced a ban the use of organophosphate pesticide methyl parathion and significant restrictions on the use of another OP, azinphos methyl, in what they called "kid's food".[47] The review process was concluded in 2006 and eliminated or modified thousands of other uses of pesticides.[48] Other legislative action has been taken to protect children from the risks of organophosphates.
Many non-governmental and research groups, as well as the EPA's Office of Inspector General, have published concerns that the review did not take into account possible neurotoxic effects on developing fetuses and children, an area of developing research. OIG report. A group of leading EPA scientists sent a letter to the chief administrator, Stephen Johnson, decrying the lack of developmental neurotoxicity data in the review process. EPA Letter EHP article New studies have shown toxicity to developing organisms during certain "critical periods" at doses much lower than those previously suspected to cause harm.[49]
Even the restrictions that did successfully pass have been controversial. For example, in 1999 the EPA restricted the use of chlorpyrifos in households (under the commercial name Dursban). However, the EPA did not limit its use in agriculture. Chlorpyrifos remains one of the most widely used pesticides.[50] This may soon change. On February 8, 2013 the EPA requested comment on a preliminary evaluation of the potential risks to children and other bystanders from volatilization of chlorpyrifos from treated crops[51]
Research
Currently, more research is being done on animal fetuses to determine the effects of OP's during critical periods of development. Due to children's decreased size, faster rate of respiration, and continuing organ development, this area is important to research. Research to determine the variability on the PON1 enzyme in humans is also currently being researched.
The use of the organophosphates in aviation lubricating oils and hydraulic fluids and its impact on health and flight safety is currently being researched. Aerotoxic syndrome is a medical condition allegedly caused by exposure to contaminated bleed air.
Purdey (1998) suggested that organophosphates, in particular Phosmet, induced the transmissible spongiform encephalopathy epidemic of BSE.[52] A European Union food safety Scientific Steering Committee examined the evidence and did not find a link.[53]
References
- 1 2 Stoller, James K.; Michota, Franklin A.; Mandell, Brian F. (2009). The Cleveland Clinic Foundation Intensive Review of Internal Medicine. Lippincott Williams & Wilkins. p. 108. ISBN 9780781790796.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Eddleston, Michael; Buckley, Nick A; Eyer, Peter; Dawson, Andrew H (February 2008). "Management of acute organophosphorus pesticide poisoning". The Lancet. 371 (9612): 597–607. doi:10.1016/S0140-6736(07)61202-1. PMID 17706760.
- 1 2 Berg, Sheri; Bittner, Edward A. (2013). The MGH Review of Critical Care Medicine. Lippincott Williams & Wilkins. p. 298. ISBN 9781451173680.
- 1 2 3 King, Andrew M.; Aaron, Cynthia K. (February 2015). "Organophosphate and Carbamate Poisoning". Emergency Medicine Clinics of North America. 33 (1): 133–151. doi:10.1016/j.emc.2014.09.010. PMID 25455666.
- ↑ Neurological Practice: An Indian Perspective. Elsevier India. 2005. p. 479. ISBN 9788181475497.
- ↑ Leibson T, Lifshitz M (2008). "Organophosphate and Carbamate Poisoning: Review of the Current Literature and Summary of Clinical and Laboratory Experience in Southern Israel". J Toxicology. 10: 767–7704.
- 1 2 3 Eskenazi B, Bradman A, Castorina R (1999). "Exposures of Children to Organophosphate Pesticides and Their Potential Adverse Health Effects". J Environmental Health Perspectives. 107: 409–419. doi:10.1289/ehp.99107s3409.
- ↑ Toxicity, Organophosphate and Carbamate at eMedicine
- 1 2 Moore C (2009). Children and Pollution: Why Scientists Disagree. Oxford University Press. pp. 109–112. ISBN 978-0-19-538666-0.
- ↑ Woodruff T, Janssen S, Guillete L, Giudice L (2010). Environmental Impacts on Reproductive Health and Fertility. Cambridge University Press. p. 109. ISBN 978-0-521-51952-6.
- ↑ Peiris-John R, Wickremasinghe R (2008). "Impact of low-level exposure to organophosphates on human reproduction and survival". Royal Society of Tropical Medicine and Hygiene. 102: 239–245. doi:10.1016/j.trstmh.2007.11.012.
- ↑ Rauh V, Arunajadai S, Horton M, et al. (2011). "Seven-year neurodevelopmental scores and prenatal exposure to chlorpyrifos, a common agricultural pesticide". Environmental Health Perspectives. 119: 1189–1195. doi:10.1289/ehp.1003160. PMC 3237355
 . PMID 21507777.
. PMID 21507777. - ↑ Bourchard M; Chevrier J; Harley K; Kogut K; Vedar M; Caldron N. Trujillo C; Johnson C; Bradman A; Barr D; Eskenazi B (1999). "Prenatal Exposure to Organophosphate Pesticides and IQ in 7-Year-Old Children". Environ Health Perspect. 119: 1189–1195. doi:10.1289/ehp.1003185. PMC 3237357
 . PMID 21507776.
. PMID 21507776. - 1 2 Eskenazi B, Harley K, Bradman A, Weltzien E, Jewell N, Barr D, Furlong C, Holland N (2004). "Association of in Utero Organophosphate Pesticide Exposure and Fetal Growth and Length of Gestation in an Agricultural Population". Environ Health Perspect. 112: 116–1124. doi:10.1289/ehp.6789.
- ↑ Rauh V, Perera F, Horton M, Whyatt R, Bansal R, Hao X, Liu J, Barr D, Slotkin T, Peterson B (2012). "Brain anomalies in children exposed prenatally to a common organophosphate pesticide". Proc Natl Acad Sci U S A. 109: 7871–7876. doi:10.1073/pnas.1203396109.
- 1 2 3 Jokanovic M, Kosanovic M (2010). "Neurotoxic effects in patients poisoned with organophosphate pesticides". Environmental Toxicology and Pharmacology. 29: 195–201. doi:10.1016/j/etap.2010.01.006.
- ↑ Freire, C., & Koifman, S. (2013). Pesticides, depression and suicide: A systematic review of the epidemiological evidence. International Journal of Hygiene and Environmental Health, 216(4), 445-460. doi:10.1016/j.ijheh.2012.12.003
- ↑ "Cholinesterase Inhibition".
- ↑ "Pesticide Application and Safety Training for Applicators of Public Health Pesticides". Archived from the original on 2010-08-29. Retrieved 2013-03-25.
- ↑ "Because some foods carry organophosphate residues".
- ↑ "Methyl Parathion Risk Management Decision". Retrieved 2013-03-25.
- ↑ "EWG's 2012 Shopper's Guide to Pesticides in Produce™". Environmental Working Group. Retrieved 2013-03-25.
- ↑ ": Health Effects of 30 Commonly Used Lawn Pesticides" (PDF).
- 1 2 3 4 Costa L, Cole T, Vitalone A, Furlong C (2005). "Measurement of paraoxonase (PON1) status as a potential biomarker of susceptibility to organophosphate toxicity". Clinica Chimica Acta. 352: 37–47. doi:10.1016/j.cccn.2004.09.019. PMID 15653099.
- ↑ "Organophosphorous Cumulative Risk Assessment 2006 Update" (PDF). US EPA Office of Pesticide Programs. Retrieved 2011-12-10.
- 1 2 Worek F, Koller M, Thiermann H, Szinicz L (2005). "Diagnostic aspects of organophosphate poisoning". J Toxicology. 214: 182–9. doi:10.1016/j.tox.2005.06.012.
- ↑ EQM Research. Test-mate Official Site Page accessed 8 Feb 2015.
- ↑ Paul L. Knechtges. May 2008 USACEHR Technical Report 0801: An Evaluation of Blood Cholinesterase Testing Methods for Military Health Surveillance
- ↑ K.D. Katz, D.E. Brooks, "Organophosphate Toxicity Workup", "MedScape", 27 Jan. 2015
- ↑ Jokanović M, Prostran M (2009). "Pyridinium oximes as cholinesterase reactivators. Structure-activity relationship and efficacy in the treatment of poisoning with organophosphorus compounds". Curr. Med. Chem. 16 (17): 2177–88. doi:10.2174/092986709788612729. PMID 19519385.
- ↑ Balali-Mood M, Shariat M (1998). "Treatment of organophosphate poisoning. Experience of nerve agents and acute pesticide poisoning on the effects of oximes". J Physiology. 92: 375–378. doi:10.1016/s0928-4257(99)80008-4.
- ↑ Rahimi R, Nikfar S, Abdollahi M (March 2006). "Increased morbidity and mortality in acute human organophosphate-poisoned patients treated by oximes: a meta-analysis of clinical trials". Hum Exp Toxicol. 25 (3): 157–62. doi:10.1191/0960327106ht602oa. PMID 16634335.
- ↑ Peter JV, Moran JL, Graham P (February 2006). "Oxime therapy and outcomes in human organophosphate poisoning: an evaluation using meta-analytic techniques". Crit. Care Med. 34 (2): 502–10. doi:10.1097/01.CCM.0000198325.46538.AD. PMID 16424734.
- ↑ Walker C (2001). Organic Pollutants: An Ecotoxicological Perspective. Taylor & Francis. pp. 186–193. ISBN 0-7484-0962-9.
- 1 2 Doctor B, Saxena A (2005). "Bioscavengers for the protection of humans against organophosphate toxicity". Chemico-Biological Interactions. 157-158: 167–171. doi:10.1016/j.cbi.2005.10.024.
- ↑ Banerjee I, Tripathi SK, Roy AS (2014). "Efficacy of pralidoxime in organophosphorus poisoning: Revisiting the controversy in Indian setting". J Postgrad Med. 60: 27–30. doi:10.4103/0022-3859.128803.
- ↑ Zoltani C, Baskin S (2002). "Organophosphate Caused Cardia Toxicity: Action Potential Dynamics in Atrial Tissue". Army Research Laboratory: 1–15.
- ↑ Morgan JP, Tulloss TC (December 1976). "The Jake Walk Blues. A toxicologic tragedy mirrored in American popular music". Ann. Intern. Med. 85 (6): 804–8. doi:10.7326/0003-4819-85-6-804. PMID 793467.
- ↑ Segalla Spencer (2011). "The 1959 Moroccan Oil Poisoning and US Cold War Disaster Diplomacy". Journal of North African Studies. 17: 315–336. doi:10.1080/13629387.2011.610118.
- ↑ Horn J, Haley R, Kurt T (1997). "Neuropsychological Correlates of Gulf War Syndrome". Archives of Clinical Neuropsychology. 12: 531–544.
- ↑ Haley R, Kurt T (Jan 1997). "Self-reported exposure to neurotoxic chemical combinations in the Gulf War: A cross-sectional epidemiologic study". Journal of the American Medical Association. 277 (3): 231–237. doi:10.1001/jama.277.3.231.
- ↑ Toomy R, Alpern R, Vasterling J, Backer D, Reda D, Lyons M, Henderson W, Kang H, Eisen S, Murphy F (2009). "Neuropsychological functioning of U.S. Gulf War veterans 10 years after the war". Journal of the International Neuropsychological Society. 15 (5): 717–29.
- ↑ https://www.theguardian.com/environment/2015/apr/20/revealed-government-knew-of-farm-poisoning-risk-but-failed-to-act
- ↑ "Pesticide Registration (PR) Notice 1988-6" (PDF). Retrieved 2013-03-28.
- ↑ "Setting Tolerances for Pesticide Residues in Foods". Retrieved 2013-03-28.
- ↑ "Food Quality Protection Act (FQPA) of 1996". Retrieved 2013-03-28.
- ↑ "Children Are at Greater Risks from Pesticide Exposure". United States Environmental Protection Agency. January 2002. Retrieved 18 February 2015.
- ↑ Janofsky, Michael. "E.P.A. Recommends Limits On Thousands of Pesticides", The New York Times, August 4, 2006, accessed April 1, 2008.
- ↑ Slotkin TA, Levin ED, Seidler FJ (May 2006). "Comparative developmental neurotoxicity of organophosphate insecticides: effects on brain development are separable from systemic toxicity". Environ. Health Perspect. 114 (5): 746–51. doi:10.1289/ehp.8828. PMC 1459930
 . PMID 16675431.
. PMID 16675431. - ↑ "Reregistration Eligibility Decision for Chlorpyrifos" (PDF). 31 July 2006.
- ↑ "Pesticide News Story: Chlorpyrifos Preliminary Volatilization Assessment Suggests Bystander Risks of Concern; EPA Requests Comment to Address Uncertainties". 2013-02-08. Retrieved 2013-03-28.
- ↑ Purdey M (February 1998). "High-dose exposure to systemic phosmet insecticide modifies the phosphatidylinositol anchor on the prion protein: the origins of new variant transmissible spongiform encephalopathies?". Med. Hypotheses. 50 (2): 91–111. doi:10.1016/S0306-9877(98)90194-3. PMID 9572563.
- ↑ "Health and Consumer Protection – Scientific Steering Committee – Outcome of discussions 18". Retrieved 2007-07-30.
| Classification | |
|---|---|
| External resources |