Noise-induced hearing loss
| Noise-induced hearing loss | |
|---|---|
 | |
| The international symbol of deafness and hearing loss | |
| Classification and external resources | |
| Specialty | Otorhinolaryngology, audiology |
| ICD-10 | Xxx.x |
| ICD-9-CM | xxx |
Noise-induced hearing loss (NIHL) is hearing impairment resulting from exposure to loud sound. People may have a loss of perception of a narrow range of frequencies, impaired cognitive perception of sound, or other impairment, including sensitivity to sound or ringing in the ears.[1]
Hearing may deteriorate gradually from chronic and repeated noise exposure, such as loud music or background noise, or suddenly, from a short high intensity noise such as a gunshot or airhorn.[1] In both types, loud sound overstimulates delicate hearing cells, leading to the permanent injury or death of the cells. Once lost, hearing cannot be restored in humans.[2] When exposure to hazards such as noise occur at work and is associated with hearing loss, it is referred to as occupational hearing loss.[3]
There are a variety of prevention strategies available to avoid or reduce hearing loss. If not prevented, hearing loss can be managed through assistive devices and cognitive therapies. Prevention is the best defense against noise-induced hearing loss. The best, first option for protecting hearing is lowering the volume of sound at its source.[4] Secondly, limiting the time of exposure to loud noise can reduce injury. Finally, physical protection from the noise can reduce its impact. Government regulations are designed to limit occupational exposure to dangerously loud noise.
The largest burden of NIHL, has been through occupational exposures; however, noise-induced hearing loss can also be due to unsafe recreational, residential, social, and military service-related noise exposures.[5] It is estimated that 15% of young people are exposed to sufficient leisure noises (i.e. concerts, sporting events, daily activities, personal listening devices, etc.) to cause NIHL.[6] There is not a limited list of noise sources that can cause hearing loss. Rather, it is important to understand that exposure to excessively high decibel levels from any sound source over time, can cause hearing loss.
Signs and symptoms
The first symptom of noise-induced hearing loss is usually difficulty hearing a conversation against a noisy background.[7] The effect of hearing loss on speech perception has two components. The first component is the loss of audibility, which is something like a decrease in overall volume. Modern hearing aids compensate this loss with amplification. However, difficulty in understanding speech represents selective frequency loss for which hearing aids and amplification do not help. This is known by different names such as “distortion,” “clarity loss,” and “Signal-to-Noise-Ratio (SNR)-loss.”[8] Consonants, due to their higher frequency, seem to be lost first.[7] For example, the letters “s” and “t” are the common letters that are difficult to hear for those with hearing loss due to them being our highest frequency sound in our language.[9] Hearing loss can affect either one or both ears. When one ear is affected it causes problems with directional hearing. Directional hearing provides the ability to determine from which direction a sound came. Lacking this ability can cause confusion within individuals who have hearing loss in one ear.[9]
Temporary and permanent
- PTS (Permanent Threshold Shift): the part of the hearing loss subsequent to an acoustic trauma that will never be recovered. PTS is measured in decibels.
- TTS (Temporary Threshold Shift): the hearing loss that will be recovered after a couple of days. Also called auditory fatigue. TTS is also measured in decibels.
TTS imperceptibly gives way to PTS.[1]
In addition to hearing loss, other external symptoms of an acoustic trauma can be:
- Tinnitus[10]
- Some pain in the ear[11]
- Hyperacusis[10]
- Dizziness or vertigo; in the case of vestibular damages, in the inner-ear[12]
Tinnitus
An estimated 50 million Americans have some degree of tinnitus in one or both ears; 16 million of them have symptoms serious enough for them to see a doctor or hearing specialist. As many as 2 million become so debilitated by the unrelenting ringing, hissing, chirping, clicking, whooshing or screeching, that they cannot carry out normal daily activities.[13]
Tinnitus is the largest single category for disability claims in the military, with hearing loss a close second.[14] The third largest category is post-traumatic stress disorder, which itself may be accompanied by tinnitus and may exacerbate it.[14]
Physiological response
The symptoms mentioned above are the external signs of the physiological response to cochlear overstimulation. Here are some elements of this response:
- Broken and "bent" hairs of the hair-cells; damaged hair-cells degeneration. In humans, dead hair-cells are never replaced; the resulting hearing loss is thus irreparable.[15]
- Inflammation of the exposed areas. This inflammation causes a bad blood flow in the exposed blood vessels (vascular stasis), and a bad oxygen supply for the liquid inside the cochlea (endolymphatic hypoxia)[16] Those noxious conditions worsen the damaged hair-cells degeneration.
- Synaptic damages, by excitotoxicity. Noise overstimulation causes an excessive release of glutamate, causing the postsynaptic bouton to swell and burst. However the neuron connection can be repaired, and the hearing loss only caused by the "wiring" (i.e. excitotoxicity) can thus be recovered within 2–3 days.[17]
Quality of life
NIHL has implications on quality of life that extend beyond related symptoms and the ability to hear. The annual disability-adjusted life years (DALYs) were estimated for noise-exposed U.S. workers.[18][20] DALYs represent the number of healthy years lost due to a disease or other health condition. They were defined by the 2013 Global Burden of Disease (GBD) Study.[19] The DALYs calculation accounts for life limitations experienced because of hearing loss as a lost portion of a healthy year of life. So the results indicate the number of healthy years lost by a group of people over a specific time period.
NIOSH used DALYs to estimate the impact of hearing loss on quality of life in the CDC Morbidity and Mortality Weekly Report article “Hearing Impairment Among Noise-Exposed Workers in the United States, 2003-2012.” It reported that 2.5 healthy years were lost each year for every 1,000 noise-exposed U.S. workers because of hearing impairment (hearing loss that impacts day-to-day activities). These lost years were shared among the 13% of workers with hearing impairment (about 130 workers out of each 1,000 workers). Mining, Construction and Manufacturing workers lost more healthy years than workers in other industry sectors; specifically and respectively in those sectors, 3.5, 3.1 and 2.7 healthy years were lost each year for every 1,000 workers.
Negative impacts
The negative impacts of NIHL on one’s ability to reciprocate communication, socialize and interact with society are largely invisible. Hearing loss, in general, is not just an issue of volume; individuals may experience difficulty in understanding what is said over the phone, when several people are talking at once, in a large space, or when the speaker’s face cannot be seen.[20] Subsequently, challenging social interactions can negatively lead to decreased self-esteem, shame, and fear. This can be more acutely felt by those who experience hearing impairment or loss earlier in life, rather than later when it is more socially accepted.[21] Such psychosocial states, regardless of age, can lead to social isolation, which is known to negatively impact one’s overall health and well-being.[22] The compounding impacts can also lead to depression,[21] especially if hearing impairment leads to tinnitus.[23] Research suggests that those with hearing impairment or loss may be at a greater risk for deterioration of quality of life,[24] as captured by a quote from Helen Keller: “Blindness cuts us off from things, but deafness cuts us off from people.”[25] Hearing impairment and loss of hearing, regardless of source or age, also limits experiencing the many benefits of sound on quality of life. In addition to the interpersonal social benefits, new studies suggest the effects of nature sounds, such as birds chirping and water, can positively affect an individual’s capacity to recover after being stressed or to increase cognitive focus.[26][27]
Quality of life questionnaire
Hearing loss is typically quantified by results from an audiogram; however, the degree of loss of hearing does not predict the impact on one’s quality of life.[28] The impact that NIHL can have on daily life and psychosocial function can be assessed and quantified using a validated questionnaire tool, such as the Hearing Handicap Inventory for the Elderly (HHIE). The HHIE is considered a “useful tool for quantifying the perceived emotional and social/situational consequences of hearing loss.”[28] The original tool was designed to test adults 65 years of age and older; however, modified versions exist. For adults the Hearing Handicap Inventory for Adults (HHIA) can be used[29] and for adolescents the modified 28-item Hearing Environments And Reflection on Quality of Life (HEAR-QL-28) can be used.[30] The HHIA, for example, is a 25-item questionnaire that asks both social and emotional-specific questions such as: Does a hearing problem cause you to avoid groups of people?” (social) and “Does a hearing problem cause you to feel frustrated when talking to members of your family?” (emotional). Response options are yes, no and sometimes.[29][31]
Cause
The ear can be exposed to short periods of sound in excess of 120 dB without permanent harm — albeit with discomfort and possibly pain; but long term exposure to sound levels over 80 dB can cause permanent hearing loss.[32]
There are two basic types of NIHL:
- NIHL caused by acoustic trauma and
- gradually developing NIHL.
Acute acoustic trauma
NIHL caused by acute acoustic trauma refers to permanent cochlear damage from a one-time exposure to excessive sound pressure. This form of NIHL commonly results from exposure to high-intensity sounds such as explosions, gunfire, a large drum hit loudly, and firecrackers.
Perceived harmfulness vs. actual harmfulness
The discomfort threshold is the loudness level from which a sound starts to be felt as "too loud" and thus painful by an individual. Industry workers tend to have a higher discomfort threshold (i.e. the sounds must be louder to feel painful than for non-industry workers), but the sound is just as harmful to their ears.[33] Industry workers often suffer from NIHL because the discomfort threshold is not a relevant indicator of the harmfulness of a sound.[33]
Gradually developing
Gradually developing NIHL refers to permanent cochlear damage from repeated exposure to loud sounds over a period of time. Unlike acoustic trauma, this form of NIHL does not occur from a single exposure to a high-intensity sound pressure level. Gradually developing NIHL can be caused by multiple exposures to excessive noise in the workplace or any source of repetitive, frequent exposures to sounds of excessive volume, such as home and vehicle stereos, concerts, nightclubs, and personal media players.
Workplace
About 22 million workers are exposed to hazardous noise, with additional millions exposed to solvents and metals that could put them at increased risk for hearing loss.[34] Occupational hearing loss is one of the most common occupational diseases. 49% of male miners have hearing loss by the age of 50.[35] By the age of 60, this number goes up to 70%.[35] Construction workers also suffer an elevated risk. A screening program focused on construction workers employed at US Department of Energy facilities found 58% with significant abnormal hearing loss due to noise exposures at work.[36] Occupational hearing loss is present in up to 33% of workers overall.[37] Occupational exposure to noise causes 16% of adult disabling hearing loss worldwide.[38]
The following is a list of occupations that are most susceptible to hearing loss:[35]
- Agriculture
- Mining
- Construction
- Manufacturing
- Utilities
- Transportation
- Military
- Musicians
- Orchestra conductors
Among musicians
Musicians, from classical orchestras to rock groups, are exposed to high decibel ranges.[39][40] Some rock musicians experience noise-induced hearing loss from their music,[41] and some studies have found that "symphonic musicians suffer from hearing impairment and that the impairment might be ascribed to symphonic music."[42]
Music-induced hearing loss is still a controversial topic for hearing researchers.[43] While some populational studies have shown that the risk for hearing loss increases as music exposure increases,[43] other studies found little to no correlation between the two.[43] Experts at the 2006 "Noise-Induced Hearing Loss in Children at Work and Play" Conference agreed that further research into this field was still required before making a broad generalization about music-induced hearing loss.[43]
Given the extensive research suggesting that industrial noise exposure can cause sensorineural hearing loss a link between hearing loss and music exposures of similar level and duration (to industrial noise) seems highly plausible. Determining which individuals or groups are at risk for such exposures may be a difficult task. Recent research suggests that despite concerns about the proliferation of personal music players, in fact discos, concerts and live music events may be more hazardous to youth's hearing.[44][45] People from ages to 6–19 have an approximately 15% rate of hearing loss.[37] Recommendations for musicians to protect their hearing have been released in 2015.[46]
Workplace standards
In the United States, the Occupational Safety and Health Administration (OSHA) describes standards for occupational noise exposure in articles 1910.95 and 1926.52. OSHA states that an employer must implement hearing conservation programs for employees if the noise level of the workplace is equal to or above 85 dB(A) for an averaged eight-hour time period.[47] OSHA also states that "exposure to impulsive or impact noise should not exceed 140 dB peak sound pressure level".[32] The National Institute for Occupational Safety and Health (NIOSH) recommends that all worker exposures to noise should be controlled below a level equivalent to 85 dBA for eight hours to minimize occupational noise induced hearing loss. NIOSH also recommends a 3 dBA exchange rate so that every increase by 3 dBA doubles the amount of the noise and halves the recommended amount of exposure time.[48] The United States Department of Defense (DoD) instruction 605512 has some differences from OSHA 1910.95 standard, for example, OSHA 1910.95 uses a 5 dB exchange rate and DoD instruction 605512 uses a 3 dB exchange rate.
There are programs that seek to increase compliance and therefore effectiveness of hearing protection rules; the programs include the use of hearing tests and educating people that loud sound is dangerous[49]
Employees are required to wear hearing protection when it is identified that their eight-hour time weighted average (TWA) is above the exposure action value of 90 dB. If subsequent monitoring shows that 85 dB is not surpassed for an eight-hour TWA, the employee is no longer required to wear hearing protection.[50]
In the European Union, directive 2003/10/EC mandates that employers shall provide hearing protection at noise levels exceeding 80 dB(A), and that hearing protection is mandatory for noise levels exceeding 85 dB(A).[51] Both values are based on 8 hours per day, with a 3 dB exchange rate.
A 2012 Cochrane review found low-quality evidence that legislation to reduce noise in the workplace was successful in reducing exposure both immediately and long-term.[38]
Mechanisms

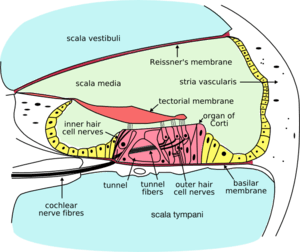
NIHL occurs when too much sound intensity is transmitted into and through the auditory system. An acoustic signal from a sound source, such as a radio, enters into the external auditory canal, and is funneled through to the tympanic membrane (eardrum). The tympanic membrane acts as an elastic diaphragm driving the ossicular chain of the middle ear system into motion. The middle ear ossicles transfer mechanical energy to the cochlea by way of the stapes footplate hammering against the oval window of the cochlea. This hammering causes the fluid within the cochlea (perilymph and endolymph) to push against the stereocilia of the hair cells, which then transmit a signal to the central auditory system within the brain. Different groups of hair cells are responsive to and conductive of different frequencies. There are two known biological mechanisms of NIHL from excessive sound intensity: damage to the hair cells and damage to the myelination or synaptic regions of auditory nerves.
Hair cell damage or death
When the ear is exposed to excessive sound levels or loud sounds over time, the overstimulation of the hair cells leads to heavy production of reactive oxygen species, leading to oxidative cell death. In animal experiments, antioxidant vitamins have been found to reduce hearing loss even when administered the day after noise exposure.[52] They were not able to fully prevent it. Damage ranges from exhaustion of the "hair" (hearing) cells in the ear to loss of those cells[47] NIHL is therefore the consequence of overstimulation of the hair cells and supporting structures. Structural damage to hair cells (primarily the outer hair cells) will result in hearing loss that can be characterized by an attenuation and distortion of incoming auditory stimuli.
During cell death ‘scars’ develop, which prevent potassium rich fluid on the endolymph from mixing with the fluid on the basal domain.[53] The fluids are kept from mixing because the potassium rich fluid is toxic to the neuronal endings and can damage hearing of the entire ear. If the endolymph fluid mixes with the fluid on the basal domain the neurons become depolarized, causing complete hearing loss. In addition to complete hearing loss, if the area is not sealed and leakage continues further tissue damage will occur. The ‘scars’ that form to replace the damaged hair cell are caused by supporting hair cells undergoing apoptosis and sealing the reticular lamina, which prevents fluid leakage.[53] The cell death of two supporting hair cells rapidly expands their apical domain, which compresses the hair cell beneath its apical domain.[53]
Nerve damage
Recent studies have investigated additional mechanisms of NIHL involving delayed or disabled electrochemical transmission of nerve impulses from the hair cell to and along the auditory nerve. In cases of extreme acute acoustic trauma, a portion of the postsynaptic dendrite (where the hair cell transfers electrochemical signal to the auditory nerve) can rupture from overstimulation, temporarily stopping all transmission of auditory input to the auditory nerve. This is known as excitotoxicity. Usually, this sort of rupture heals within about five days, resulting in functional recovery of that synapse. While healing, an over-expression of glutamate receptors can result in temporary tinnitus, or ringing in the ears. Repeated ruptures at the same synapse may eventually fail to heal, leading to permanent hearing loss.[54]
Acoustic over-exposure can also result in decreased myelination at specific points on the auditory nerve. Myelin, an insulating sheath surrounding nerve axons, expedites electrical impulses along nerves throughout the nervous system. Thinning of the myelin sheath on the auditory nerve significantly slows the transmission of electrical signals from hair cell to auditory cortex, reducing comprehension of auditory stimuli by delaying auditory perception, particularly in noisy environments.[55]
Individual susceptibility towards noise
There appear to be large differences in individual susceptibility to NIHL.[56] The following factors have been implicated:
- missing acoustic reflex[15]
- previous sensorineural hearing loss[57]
- a bad general health state: bad cardiovascular function, insufficient intake of oxygen, a high platelet aggregation rate; and most importantly, a high viscosity of the blood[15]
- cigarette smoking[57]
- exposure to ototoxic chemicals (medication or environmental chemicals that can damage the ear), including certain solvents and heavy metals[38][57][58]
- type 2 diabetes[57]
Diagnosis

Both NIHL caused by acoustic trauma and gradually-developed-NIHL can often be characterized by a specific pattern presented in audiological findings. NIHL is generally observed to affect a person's hearing sensitivity in the higher frequencies, especially at 4000 Hz. "Noise-induced impairments are usually associated with a notch-shaped high-frequency sensorineural loss that is worst at 4000 Hz, although the notch often occurs at 3000 or 6000 Hz, as well".[47] Doctoral students at the University of Iowa have termed this notch, specific to a noise-induced etiology, a "muna." The symptoms of NIHL are usually presented equally in both ears.[47]
This typical 4000 Hz notch is due to the transfer function of the ear.[15] Indeed, as any object facing a sound, the ear acts as a passive filter (-although the inner ear is not an absolute passive filter, as the outer hair cells provide active mechanisms). A passive filter is a low pass : the high frequencies are more absorbed by the object, as high frequencies impose a higher pace of compression-decompression to the object. Thus, the high frequency harmonics of a sound are more harmful to the inner-ear.
However, not all audiological results from people with NIHL match this typical notch. Often a decline in hearing sensitivity will occur at frequencies other than at the typical 3000–6000 Hz range. Variations arise from differences in people's ear canal resonance, the frequency of the harmful acoustic signal, and the length of exposure.[59] As harmful noise exposure continues, the commonly affected frequencies will broaden and worsen in severity.[47] "NIHL usually occurs initially at high frequencies (3, 4, or 6 kHz), and then spreads to the low frequencies (0.5, 1, or 2 kHz)".[60]
Prevention

NIHL can be prevented through the use of simple, widely available, and economical tools. This includes but is not limited to personal noise reduction through the use of ear protection (i.e. earplugs and earmuffs), education, and hearing conservation programs. For the average person, there are three basic things that can be kept in mind to reduce NIHL, “walk away, turn it down, protect your ears.”[61]
Personal noise reduction devices
Personal noise reduction devices can be passive, active or a combination. Passive ear protection includes earplugs or earmuffs which can block noise up to a specific frequency. Earplugs and earmuffs can provide the wearer with 10 dB to 40 dB of attenuation.[62] However, use of earplugs is only effective if the users have been educated and use them properly; without proper use, protection falls far below manufacturer ratings.[63] Higher consistency of performance has been found with custom-molded earplugs. Because of their ease of use without education, and ease of application or removal, earmuffs have more consistency with both compliance and noise attenuation. Active ear protection (electronic pass-through hearing protection devices or EPHPs) electronically filter out noises of specific frequencies or decibels while allowing the remaining noise to pass through.[62]
Education
Education is key to prevention. Before hearing protective actions will take place, a person must understand they are at risk for NIHL and know their options for prevention. Hearing protection programs have been hindered by people not wearing the protection for various reasons, including the desire to converse, uncomfortable devices, lack of concern about the need for protection, and social pressure against wearing protection.[49] Although youth are at risk for hearing loss, one study found that 96.3% of parents did not believe their adolescents were at risk, and only 69% had talked to their children about hearing protection; those aware of NIHL risks were more likely to talk to their teens.[64]
A systematic review of the effectiveness of interventions to promote the use of hearing protection devices such as earplugs and earmuffs among workers found that tailored interventions improve the average use of such devices when compared with no intervention.[65] Tailored interventions involve the use of communication or other types of interventions that are specific to an individual or a group and aim to change behavior.[65] Mixed interventions such as mailings, distribution of hearing protection devices, noise assessments, and hearing testing are also more effective in improving the use of hearing protection devices compared with hearing testing alone.[65] Programs that increased the proportion of workers wearing hearing protection equipment did reduce overall hearing loss.[38] However, a 2012 Cochrane review found that hearing loss prevention programs have not shown as much success with educational messages as with use of hearing protective devices; better implementation and reinforcement of these programs are needed.[66]
Personal listening devices
A 2012 study looked at the safety of using personal listening devices as well as the comparative safety of earbuds, in-ear earphones, and supra-aural earphones (over the ear).[67] The study found that since supra-aural earphones blocked out background noise better than the other earphones, sound was listened to at a quieter, and safer volume. Ear buds blocked the least amount of environmental noise and seemed to result in the most noise pressure. Recommendations for safe use of personal listening devices included: keeping the volume at the lowest possible setting, taking care to keep volume below 50% even in loud settings such as buses or airplanes, and selecting an earphone that is better at attenuating environmental noise.[67]
Hearing conservation programs
Workers in general industry who are exposed to noise levels above 85 dBA are required by the Occupational Safety and Health Administration (OSHA) to be in a hearing conservation program (HCP), which includes noise measurement, noise control, periodic audiometric testing, hearing protection, worker education, and record keeping. Twenty-four states, Puerto Rico, and the U.S. Virgin Islands have OSHA-approved state plans and have adopted their own standards and enforcement policies. Most of these state standards are identical to those of federal OSHA. However, some states have adopted different standards or may have different enforcement policies. Most health and safety regulations are designed to keep damage risk within “acceptable limits” — that is, some people are likely to incur a hearing loss even when exposed to less than the maximum daily amount of noise specified in a regulation. Hearing conservation programs in other arenas (schools, military) have become more common, and it has been established that unsafe listening behaviors, such as listening to loud noise for extended periods of time without protection, persist despite knowledge of potential hearing loss effects.[68][69]
However, it is understood that HCPs are designed to change behavior, which is known to be a complex issue that requires a multi-faceted approach. According to Keppler et al. in their 2015 study of such programming, they cite the necessary attitude change towards the susceptibility of risk and degree of severity of hearing loss. Among young adults, the concept of severity is most crucial because it has been found that behavior change may not occur unless an individual experiences NIHL or similarly related NIHL tinnitus,[69] furthering warranting a multi-pronged approach based on hearing conservation programming and education.
Other initiatives
There are a variety of public awareness programs as well as available curricula to teach awareness messages becoming available. One such program is Dangerous Decibels, whose mission is to “significantly reduce the prevalence of noise induced hearing loss and tinnitus through exhibits, education and research.[61] We’re hEAR for You is a small non-profit that distributes information and ear plugs at concert and music festival venues.[70] The Buy Quiet program was created to combat occupational noise exposures by promoting the purchase of quieter tools and equipment and encourage manufacturers to design quieter equipment.[71] The National Institute for Occupational Safety and Health partnered with the National Hearing Conservation Association in 2007 to establish the Safe-in-Sound Excellence and Innovation in Hearing Loss Prevention Awards to recognize organizations that are successfully implementing hearing loss prevention concepts into their daily routines.[72]
Pharmacalogical
There is evidence that hearing loss can be minimized by taking high doses of magnesium for a few days, starting as soon as possible after exposure to the loud noise.[73][74] A magnesium-high diet also seems to be helpful as an NIHL-preventative if taken in advance of exposure to loud noises.[75] Consuming sizable amounts of magnesium can be potentially harmful, so this treatment should be followed with caution.[76]
Sound or stress training
Despite different people having different thresholds for what noises are painful, this pain threshold had no correlation with which noises cause hearing damage. The ear can not get more resistant to noise harmfulness by training it to noise. The cochlea is partially protected by the acoustic reflex, but being frequently exposed to noise does not lower the reflex threshold.[33] It had been observed that noise conditioning (i.e. exposure to loud non-traumatizing noise) several hours prior to the exposure to traumatizing sound level, significantly reduced the damages inflicted to the hair-cells.[77] The same “protective effect" was also observed with other stressors such as heat-shock conditioning[78] and stress (by restraint) conditioning.[79] This “protective effect" only happens if the traumatizing noise is presented within an optimum interval of time after the sound-conditioning session (-24 hours for a 15 min. sound-conditioning; no more protection after 48 hours[80]).
This “protective effect” had long been thought to involve the active mechanisms of the outer hair cells and the efferent system commanding them.[15] The contractile effect of the outer hair cells, activated by the efferent nervous system has been proven to provide a protective effect against acoustic trauma.[81]
However, a 2006 study revealed a different protective mechanism for stress conditioning.[82] The study revealed that the stressor (sound, heat, or stress) conditioning increases the receptibility to glucocorticoid, a kind of anti-inflammatory hormone. The effects of glucocorticoid thus mitigate the inflammation from an acoustic trauma that can lead to hearing loss. In fact, high doses of corticoids are often prescribed by physicians after an acoustic-trauma[83] in order to mitigate the inflammatory response.
Summarized, sound (or other stressor) conditioning is a pre-emptive medication against cochlea inflammation. It does not make the ear more resistant to noise. It reduces the inflammation caused by the acoustic trauma, which would cause subsequent damages to hair cells. While an anti-inflammatory medication would increase the quantity of anti-inflammatory hormone in the whole body, noise conditioning increases the number of receptors for the anti-inflammatory hormone, and only in the areas where it is much needed (i.e. cochlea).
Physiological response
- stressor (noise, heat shock or stress) conditioning activates hormonal glands: the HPA axis. Note that the HPA axis is associated to the immune system[84]
- this HPA axis activation results in the up regulation of glucocorticoid receptors (GR) in the cochlea and the paraventricular nucleus (PVN) of the hypothalamus. Note that the glucocorticoid hormone is a kind of immune-reaction-inhibitor, including the inflammation reaction.
- This up regulation of GR thus prevents GR down regulation induced by acoustic trauma
- The protective effect of noise-conditioning is blocked by adrenalectomy or pharmacological treatment with RU486+ metyrapone (a glucocorticoid receptor antagonist).
Treatment
Treatment options that offer “cures” for NIHL are under research and development. Currently there are no commonly used cures, but rather assistive devices and therapies to try and manage the symptoms of NIHL.
Acute acoustic trauma
Several clinical trials have been conducted to treat temporary NIHL occurring after a traumatic noise event, such as a gunshot or firework. In 2007, individuals with acute acoustic trauma after firecracker exposure were injected intratympanically with a cell permeable ligand, AM-111. The trial found AM-111 to have a therapeutic effect on at least 2 cases of those with acute trauma.[85] Treatment with a combination of prednisolone and piracetam appeared to rescue patients with acute trauma after exposure to gunshots. However, those who received the treatment within an hour of exposure had higher rates of recovery and significantly lower threshold shifts compared to those who received treatment after 1 hour.[86]
Additionally, clinical trials using antioxidants after a traumatic noise event to reduce reactive oxygen species have displayed promising results. Antibiotic injections with allopurinol, lazaroids, α-D-tocopherol, and mannitol were found to reduce the threshold shift after noise exposure.[87] Another antioxidant, Ebselen, has been shown to have promising results for both TTS and PTS.[88] Ebselen mimics gluthathione peroxide, an enzyme that has many functions, including scavenging hydrogen peroxide and reactive oxygen species.[89] After noise exposure, gluthathione peroxide decreases in the ear. An oral administration of ebselen in both preclinical tests on guinea pigs and human trials indicate that noise induced TTS and PTS was reduced.[88]
Gradually occurring NIHL
At the present time, no established clinical treatments exist to reverse the effects of permanent NIHL.[90] However, current research for the possible use of drug and genetic therapies look hopeful.[91] In addition, management options such as hearing aids and counseling exist.
Many studies have been conducted looking at regeneration of hair cells in the inner ear. While hair cells are generally not replaced through cell regeneration,[92] mechanisms are being studied to induce replacement of these important cells.[93] One study involves the replacement of damaged hair cells with regenerated cells, via the mechanism of gene transfer of atonal gene Math1 to pluripotent stem cells within the inner ear.[94] Other atonal genes are being studied to induce regeneration of hair cells in the inner ear.[92]
Management
For people living with NIHL, there are several management options that can improve the ability to communicate including counseling and the use of hearing aids and FM systems. The prognosis has improved with the recent advancements in digital hearing aid technology, such as directional microphones, open-fit hearing aids, and more advanced algorithms. Annual audiological evaluations are recommended to monitor any changes in a patient's hearing and to modify hearing-aid prescriptions.
A systematic-review conducted by the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults found the use of hearing aids to increase quality of life. The review pertained to adults who experienced sensorineural hearing loss, which can be caused by excessive, loud noise.[95]
Epidemiology
Currently, the World Health Organization estimates that nearly 360 million people suffer from moderate to profound hearing loss from all causes.[96] Incidence of hearing loss has traditionally been attributed to occupational or firearm-related exposure, however, more recent research suggests that the trend is shifting as prevalence rates increase amongst children and adolescents is increasing.[97][98] According to a 2015 review, “Hearing loss due to recreational exposure to loud sounds” by the WHO World Health Organization (WHO), an estimated 1.1 billion young people may be at risk for hearing loss caused by unsafe listening practices.[99] The over-exposure to excessive loud noise is attributed to recreational exposure, such as the use of personal audio devices with music at high volumes for long durations raises, or social settings such as bars, entertainment and sporting events.[99][100]
A review of data from the National Health and Nutrition Examination Survey in the United States found that the prevalence of high frequency hearing loss, which can be noise-induced, among adolescent 12–19 years old increased significantly from 3.5% to 5.3% from 1994 until 2006, which equates to 1 in 20 children in the U.S.[98] Although research is still limited, it suggests that increased exposure to loud noise through personal listening devices is a risk factor to this type of acquired hearing loss.[99][101] The ubiquitous use of smartphones across the world is increasing at a rate “faster than our ability to assess their potential health consequences.”[97] Despite limited research, it is documented that 90% young adults across U.S. and European surveys have reported use of personal devices for several hours a day at maximum volume. At times, this sound level can be likened to a jet engine, exceeding 120 decibels.[97] Recent research suggests stronger correlations found between extended duration and/or elevated usage of personal listening devices and hearing loss.[68]
Non-occupational noise exposure is not regulated or governed in the same manner as occupational noise exposure; therefore prevention efforts rely heavily on education awareness campaigns and public policy. The WHO cites that nearly half of those affected by hearing loss could have been prevented through primary prevention efforts such as:
“reducing exposure (both occupational and recreational) to loud sounds by raising awareness about the risks; developing and enforcing relevant legislation; and encouraging individuals to use personal protective devices such as earplugs and noise-cancelling earphones and headphones.”[96]
See also
Medical
- Sensorineural hearing loss
- Auditory fatigue
- Tinnitus
- Health effects from noise
- Hearing aid
- Hearing loss
- Occupational hearing loss
- Ototoxicity
General
- Noise
- Noise pollution
- Noise regulation
- Noise control
- Environmental noise
Organizations and awareness-raising initiatives
- Don't Lose The Music
- H.E.A.R.
- Safe-In-Sound Award
- Youth hearing conservation programs
- Hearing conservation program
Noise from power sources
References
- 1 2 3 Alberti, PW (29 February 1992). "Noise induced hearing loss." (PDF). BMJ (Clinical research ed.). 304 (6826): 522. doi:10.1136/bmj.304.6826.522. PMC 1881413
 . PMID 1559054.
. PMID 1559054. - ↑ Henderson D, Hamernik, RP, Dosanjh DS, Mills, JH (1976). Noise-induced hearing loss. New York: Raven. pp. 41–68.
- ↑ National Institute for Occupational Safety and Health, CDC (1996). Preventing Occupational Hearing Loss - A Practical Guide. Cincinnati: DHHS- 96-110. pp. iii.
- ↑ http://www.cdc.gov/niosh/topics/noisecontrol/
- ↑ Saunders, GH; Griest, SE (2009). "Hearing loss in veterans and the need for hearing loss prevention programs". Noise & Health. 11 (14): 14–21. doi:10.4103/1463-1741.45308. PMID 19265249.
- ↑ Carter, L; Williams, W; Black, A (2014). "The leisure-noise dilemma: hearing loss or hearsay? What does the literature tell us?". Ear and Hearing. 35: 491–505. doi:10.1097/01.aud.0000451498.92871.20.
- 1 2 Agius, B. "Noise induced hearing loss". Health, Work & Environment.
- ↑ Phatak, Sandeep A; Yoon, Yang-soo; Gooler, David M; Allen, Jont B (November 2009). "Consonant recognition loss in hearing impaired listeners". J Acoust Soc Am. 126 (5): 2683–2694. doi:10.1121/1.3238257. PMC 2787079
 . PMID 19894845.
. PMID 19894845. - 1 2 Lowth, Mary (2013). "Hearing Problems". Patient.
- 1 2 Temmel, AF; Kierner, AC; Steurer, M; Riedl, S; Innitzer, J (12 November 1999). "Hearing loss and tinnitus in acute acoustic trauma.". Wiener klinische Wochenschrift. 111 (21): 891–3. PMID 10599152.
- ↑ Axelsson, A.; Hamernik, R. P. (January 1987). "Acute acoustic trauma". Acta Oto-laryngologica. 104 (3-4): 225–233. doi:10.3109/00016488709107322.
- ↑ Raghunath, G; Suting, LB; Maruthy, S (2012). "Vestibular Symptoms of Factory Workers Subjected to Noise for a Long Period." (PDF). The International Journal of Occupational and Environmental Medicine. 3: 136–144.
- ↑ Adoga, AA; Obindo, TJ (2013). The Association between tinnitus and mental illness, mental disorders - Theoretical and Empirical Perspectives. InTech. ISBN 978-953-51-0919-8.
- 1 2 US Department of Veterans Affairs. "New Treatment Options for Tinnitus Sufferers".
- 1 2 3 4 5 Dancer, Armand (1991). "Le traumatisme acoustique" (PDF). médecine/sciences (in French). 7: 357–367. doi:10.4267/10608/4361.
- ↑ Misrahy, G. A. (1958). "Genesis of Endolymphatic Hypoxia Following Acoustic Trauma". The Journal of the Acoustical Society of America. 30 (12): 1082. doi:10.1121/1.1909465.
- ↑ Pujol, Rémy. "Acoustic trauma". Journey into the world of hearing. Retrieved 12 July 2015.
- ↑ Masterson, Elizabeth A.; Bushnell, P. Timothy; Themann, Christa L.; Morata, Thais C. (2016-01-01). "Hearing Impairment Among Noise-Exposed Workers — United States, 2003–2012". MMWR. Morbidity and Mortality Weekly Report. 65 (15): 389–394. doi:10.15585/mmwr.mm6515a2. ISSN 0149-2195.
- ↑ Vos, Theo; Barber, Ryan M; Bell, Brad; Bertozzi-Villa, Amelia; Biryukov, Stan; Bolliger, Ian; Charlson, Fiona; Davis, Adrian; Degenhardt, Louisa (2015-08-22). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". The Lancet. 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. ISSN 0140-6736.
- ↑ Dewane, C (2010). "Hearing loss in older adults- its effect on mental health". Social Work Today. 10 (4): 18.
- 1 2 Tambs, K (2004). "Moderate effects of hearing loss on mental health and subjective well-being: results from the Nord-Trøndelag Hearing Loss Study". Psychosomatic Medicine. 66: 776–782. doi:10.1097/01.psy.0000133328.03596.fb. PMID 15385706.
- ↑ Hawton, A; Green, C; Dickens, AP (2011). "The impact of social isolation on the health status and health-related quality of life in older people". Quality of Life Research. 20: 57–67. doi:10.1007/s11136-010-9717-2. PMID 20658322.
- ↑ Chen, J; Lian, J; Ou, J; Cai, W (2013). "Mental health in adults with sudden sensorineural hearing loss: an assessment of depressive symptoms and its correlates". Journal of psychosomatic research. 75: 72–74. doi:10.1016/j.jpsychores.2013.03.006. PMID 23751242.
- ↑ Gopinath, B; Schneider, J; Hickson, L (2012). "Hearing handicap, rather than measured hearing impairment, predicts poorer quality of life over 10 years in older adults". Mautritas. 72 (146): 146–51. doi:10.1016/j.maturitas.2012.03.010. PMID 22521684.
- ↑ Hearing Loss Association of America. "Hearing Loss and relationships". Hearing Loss Association of America.
- ↑ Alvarsson, JJ; Wiens, S; Nilsson, ME (2010). "Stress recovery during exposure to nature sound and environmental noise". International Journal of Environmental Research and Public Health. 7: 1036–1046. doi:10.3390/ijerph7031036. PMC 2872309
 . PMID 20617017.
. PMID 20617017. - ↑ Ratcilffe, E; Gatersleben, B; Sowden, PT (2013). "Bird sounds and their contributions to perceived attention restoration and stress recovery". Journal of Environmental Psychology. 36: 221–228. doi:10.1016/j.jenvp.2013.08.004.
- 1 2 Newman, CW; Weinstein, BE; Jacobson, GP; Hug, GA (1990). "The hearing handicap inventory for adults: psychometric adequacy and audiometric correlates". Ear Hear. 11 (6): 430–433. doi:10.1097/00003446-199012000-00004. PMID 2073976.
- 1 2 Newman, CW; Weinstein, BE; Jacobson, GP; Hug, GA (1991). "Test-retest reliability of the hearing handicap inventory for adults". Ear Hear. 12 (5): 355–357. doi:10.1097/00003446-199110000-00009. PMID 1783240.
- ↑ Rachakonda, T; Jeffe, DB; Shin, JJ (2014). "Validity, discriminative ability, and reliability of the hearing-related quality of life questionnaire for adolescents". The Laryngoscope. 124 (570): 578. doi:10.1002/lary.24336. PMC 3951892
 . PMID 23900836.
. PMID 23900836. - ↑ "Hearing Handicap Inventory for Adults (HHIA)" (PDF). Academy of Doctors of Audiology. Retrieved 2015. Check date values in:
|access-date=(help) - 1 2 OSHA 29 CFR 1910.95(b)(2)
- 1 2 3 W. Niemeyer (1971). "Relations between the Discomfort Level and the Reflex Threshold of the Middle Ear Muscles". Internal journal of audiology. 10: 172–176. doi:10.3109/00206097109072555.
- ↑ Tak, SangWoo; Davis, Rickie R.; Calvert, Geoffrey M. (2009-05-01). "Exposure to hazardous workplace noise and use of hearing protection devices among US workers—NHANES, 1999–2004". American Journal of Industrial Medicine. 52 (5): 358–371. doi:10.1002/ajim.20690. ISSN 1097-0274.
- 1 2 3 "Work-Related Hearing Loss". National Institute for Occupational Safety and Health. 2001.
- ↑ "The Construction Chart Book: The US Construction Industry and its Workers" (PDF). CPWR. Retrieved 12 June 2013.
- 1 2 Ehlers, Janet; Graydon, Pamela S. (11 October 2012). "Even a Dummy Knows October is Protect Your Hearing Month". National Institute for Occupational Safety and Health (NIOSH). Retrieved 22 January 2015.
- 1 2 3 4 Verbeek, Jos H.; Kateman, Erik; Morata, Thais C.; Dreschler, Wouter A.; Mischke, Christina (2012). "Interventions to prevent occupational noise-induced hearing loss". The Cochrane Database of Systematic Reviews. 10: CD006396. doi:10.1002/14651858.CD006396.pub3. ISSN 1469-493X. PMID 23076923.
- ↑ Jansson, E; Karlsson, K (1983). "Sound levels recorded within the symphony orchestra and risk criteria for hearing loss". Scandinavian audiology. 12 (3): 215–21. doi:10.3109/01050398309076249. PMID 6648318.
- ↑ Maia, Juliana Rollo Fernandes; Russo, Ieda Chaves Pacheco (2008). "Estudo da audição de músicos de rock and roll" [Study of the hearing of rock and roll musicians]. Pró-Fono Revista de Atualização Científica (in Portuguese). 20 (1): 49–54. doi:10.1590/S0104-56872008000100009. PMID 18408864.
- ↑ "Rock and Roll Hard of Hearing Hall of Fame". Guitar Player. 2006. Archived from the original on 2009-03-04.
- ↑ Ostri, B.; Eller, N.; Dahlin, E.; Skylv, G. (1989). "Hearing Impairment in Orchestral Musicians". International Journal of Audiology. 18 (4): 243–9. doi:10.3109/14992028909042202.
- 1 2 3 4 Morata, Thais C. (2007). "Young people: Their noise and music exposures and the risk of hearing loss". International Journal of Audiology. 46 (3): 111–2. doi:10.1080/14992020601103079. PMID 17365063.
- ↑ Fligor, B. J. (2009). "Risk for Noise-Induced Hearing Loss from Use of Portable Media Players: A Summary of Evidence Through 2008". Perspectives on Audiology. 5: 10. doi:10.1044/poa5.1.10.
- ↑ Williams, W (2005). "Noise exposure levels from personal stereo use". International journal of audiology. 44 (4): 231–6. doi:10.1080/14992020500057673. PMID 16011051.
- ↑ NIOSH [2015]. Reducing the risk of hearing disorders among musicians. By Kardous C, Themann C, Morata T, Reynolds J, Afanuh S Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. DHHS (NIOSH) Publication No. 2015–184. http://www.cdc.gov/niosh/docs/wp-solutions/2015-184/pdfs/2015-184.pdf
- 1 2 3 4 5 Gelfand, S. (2001). Auditory System and Related Disorders. Essentials of Audiology (2nd ed.). New York: Thieme. p. 202.
- ↑ "Occupational Noise Exposure". Centers for Disease Control and Prevention. June 1998.
- 1 2 Fausti, SA; Wilmington, DJ; Helt, PV; Helt, WJ; Konrad-Martin, D (2005). "Hearing health and care: The need for improved hearing loss prevention and hearing conservation practices". Journal of rehabilitation research and development. 42 (4 Suppl 2): 45–62. doi:10.1682/JRRD.2005.02.0039. PMID 16470464.
- ↑ "Hearing Conservation". Occupational Safety & Health Administration. 2002.
- ↑ Directive 2003/10/EC of the European Parliament and of the Council of 6 February 2003 on the minimum health and safety requirements regarding the exposure of workers to the risks arising from physical agents (noise)
- ↑ Yamasoba, Tatsuya; Nuttall, Alfred L; Harris, Craig; Raphael, Yehoash; Miller, Josef M (1998). "Role of glutathione in protection against noise-induced hearing loss". Brain Research. 784 (1–2): 82–90. doi:10.1016/S0006-8993(97)01156-6. PMID 9518561.
- 1 2 3 Yehoash, Raphael (2002). "Cochlear pathology, sensory cell death and regeneration". British Medical Bulletin. 63 (1): 25–38. doi:10.1093/bmb/63.1.25. PMID 12324382.
- ↑ Pujol, R; Puel, JL (1999). "Excitotoxicity, synaptic repair, and functional recovery in the mammalian cochlea: a review of recent findings". Ann NY Acad Sci. 28 (884): 249–254. doi:10.1111/j.1749-6632.1999.tb08646.x. PMID 10842598.
- ↑ Brown, AM; Hamann, M (2014). "Computational modeling of the effects of auditory nerve dysmyelination". Front. Neuroanat. 8 (73). doi:10.3389/fnana.2014.00073. PMC 4117982
 . PMID 25136296.
. PMID 25136296. - ↑ WHEELER, D.E. (March 1950). "NOISE-INDUCED HEARING LOSS". Arch Otolaryngol. 51: 344–355. doi:10.1001/archotol.1950.00700020366006.
- 1 2 3 4 OiSaeng Hong; Madeleine J. Kerr; Gayla L. Poling; Sumitrajit Dhar (April 2013). "Understanding and preventing noise-induced hearing loss". Elsevier. 59 (4): 110–118. doi:10.1016/j.disamonth.2013.01.002.
- ↑ Johnson AC and Morata, TC (2010). Occupational exposure to chemicals and hearing impairment. The Nordic Expert Group for Criteria Documentation of Health Risks from Chemicals. Gothenburg, Sweden: University of Gothenburg, Arbete och Hälsa 44(4). pp. 1–177. ISBN 978-91-85971-21-3.
- ↑ Rösler, G (1994). "Progression of hearing loss caused by occupational noise". Scandinavian audiology. 23 (1): 13–37. doi:10.3109/01050399409047483. PMID 8184280.
- ↑ Chen, JD; Tsai, JY (2003). "Hearing loss among workers at an oil refinery in Taiwan". Archives of Environmental Health. 58 (1): 55–8. doi:10.3200/AEOH.58.1.55-58. PMID 12747520.
- 1 2 Johnson, M; Martin, WH. "Dangerous Decibels Educator Resource Guide". Dangerous Decibels. Oregon Health and Science University.
- 1 2 Rajgurur, R (2013). "Military aircrew and noise-induced hearing loss: prevention and management". Aviation, Space, and Environmental Medicine. 84: 1268–1276. doi:10.3357/ASEM.3503.2013.
- ↑ Chen, JD; Tsai, JY (January 2003). "Hearing loss among workers at an oil refinery in Taiwan". Archives of Environmental Health. 58 (1): 55–58. doi:10.3200/AEOH.58.1.55-58. PMID 12747520.
- ↑ Clark, SJ; Davis, MM; Paul, IM; Sekhar, DL; Singer, DC (2014). "Parental Perspectives on Adolescent Hearing Loss Risk and Prevention". JAMA Otolaryngology-Head and Neck Surgery. 140: 22–28. doi:10.1001/jamaoto.2013.5760.
- 1 2 3 El Dib, RP; Mathew, JL; Martins, RH (Apr 18, 2012). "Interventions to promote the wearing of hearing protection". Cochrane database of systematic reviews (Online). 4: CD005234. doi:10.1002/14651858.CD005234.pub5. PMID 22513929.
- ↑ Verbeek JH, Kateman E, Morata TC, Dreschler WA, Mischke C. Interventions to prevent occupational noise-induced hearing loss. INT J AUDIOL. 2014 MAR; 53 SUPPL 2:S84-96. DOI: 10.3109/14992027.2013.857436. http://ONLINELIBRARY.WILEY.COM/DOI/10.1002/14651858.CD006396.PUB3/ABSTRACT
- 1 2 Breinbauer, HA; Anabalon, JL; Gutierrez, D; Olivares, C; Caro, J (2012). "Output capabilities of personal music players and assessment of preferred listening levels of test subjects: Outlining recommendations for preventing music-indused hearing loss". The Laryngoscope. 122: 2549–2556. doi:10.1002/lary.23596.
- 1 2 Ivory, R; Kane, R; Diaz, RC (2014). "Noise-induced hearing loss: a recreational noise perspective". Current opinion in otolarynology & head and neck surgery. 22: 394–8. doi:10.1097/moo.0000000000000085. PMID 25101942.
- 1 2 Keppler, H; Ingeborg, D; Bart, V; Sofie, D (2015). "The effects of a hearing education program on recreational noise exposure, attitudes and beliefs toward noise, hearing loss, and hearing protector devices in young adults.". Noise Health. 17: 253–62.
- ↑ "Mission". We're hEAR for you.
- ↑ "Buy Quiet". NIOSH. December 5, 2014. Retrieved October 28, 2015.
- ↑ "Safe-in-Sound Excellence and Innovation in Hearing Loss Prevention Awards".
- ↑ Gordin, A; Goldenberg, D; Golz, A; Netzer, A; Joachims, HZ (2002). "Magnesium: A new therapy for idiopathic sudden sensorineural hearing loss". Otology & Neurotology. 23 (4): 447–51. doi:10.1097/00129492-200207000-00009. PMID 12170143.
- ↑ Nelson, T.J. (December 4, 2009). "Noise-induced hearing loss".
- ↑ Scheibe, F; Haupt, H; Ising, H; Cherny, L (2002). "Therapeutic effect of parenteral magnesium on noise-induced hearing loss in the guinea pig". Magnesium Research. 15 (1–2): 27–36. PMID 12030420.
- ↑ "Magnesium". A.D.A.M., Inc. June 17, 2011.
- ↑ Canlon, Barbara; Fransson, Anette (April 1995). "Morphological and functional preservation of the outer hair cells from noise trauma by sound conditioning". Hearing Research. 84 (1-2): 112–124. doi:10.1016/0378-5955(95)00020-5.
- ↑ Yoshida, N; Kristiansen, A; Liberman, MC (15 November 1999). "Heat stress and protection from permanent acoustic injury in mice". The Journal of Neuroscience. 19 (22): 10116–24. PMID 10559419.
- ↑ Wang, Y; Liberman, MC (March 2002). "Restraint stress and protection from acoustic injury in mice". Hearing research. 165 (1-2): 96–102. doi:10.1016/s0378-5955(02)00289-7. PMID 12031519.
- ↑ Yoshida, N; Liberman, MC (October 2000). "Sound conditioning reduces noise-induced permanent threshold shift in mice". Hearing research. 148 (1-2): 213–9. doi:10.1016/s0378-5955(00)00161-1. PMID 10978838.
- ↑ Patuzzi, RB; Thompson, ML (1991). "Cochlear efferent neurones and protection against acoustic trauma: Protection of outer hair cell receptor current and interanimal variability". Hearing Research. 54: 45–58. doi:10.1016/0378-5955(91)90135-V.
- ↑ Tahera, Yeasmin; Meltser, Inna; Johansson, Peter (January 2007). "Sound conditioning protects hearing by activating the hypothalamic-pituitary-adrenal axis". Neurobiology of Disease. 25 (1): 189–197. doi:10.1016/j.nbd.2006.09.004.
- ↑ Casanovaa, F; Saroulb, N; Nottetc, J.B (2010). "Acute acoustic trauma: a study about treatment and prevention including 111 military doctors" (PDF). Pratique médico-militaire.
- ↑ Savastano, S; Tommaselli, AP; Valentino, R; Scarpitta, MT; D'Amore, G; Luciano, A; Covelli, V; Lombardi, G (August 1994). "Hypothalamic-pituitary-adrenal axis and immune system.". Acta neurologica. 16 (4): 206–13. PMID 7856475.
- ↑ Suckfuell, M; Canis, M; Strieth, S (2007). "Intratympanic treatment of acute acoustic trauma with a cell-permeable JNK ligand: a prospective randomized phase I/II study". Acta Otolaryngol. 127 (9): 938–42. doi:10.1080/00016480601110212.
- ↑ Psillas, G; Pavlidis, P; Karvelis, I (2008). "Potential efficacy of early treatment of acute acoustic trauma with steroids and piracetam after gunshot noise". Eur Arch Otorhinolaryngol. 265 (12): 1465–1469. doi:10.1007/s00405-008-0689-6.
- ↑ Prasher, D (1998). "New strategies for prevention and treatment of noise-induced hearing loss.". The Lancet. 352 (9136): 1240–2. doi:10.1016/S0140-6736(05)70483-9.
- 1 2 Lynch, ED; Kil, J (2005). "Compounds for the prevention and treatment of noise-induced hearing loss". Drug Discovery Today. 10 (19): 1291–8. doi:10.1016/s1359-6446(05)03561-0.
- ↑ Satheeshkumar, K; Mugesh, G (2011). "Synthesis and Antioxidant Activity of Peptide-Based Ebselen Analogues". Chem. Eur. J. 17 (17): 4849–57. doi:10.1002/chem.201003414.
- ↑ Oishi, N; Schacht, J (2011). "Emerging treatments for noise-induced hearing loss". Expert opinion on emerging drugs. 16 (2): 235–245. doi:10.1517/14728214.2011.552427. PMC 3102156
 . PMID 21247358.
. PMID 21247358. - ↑ "Noise-Induced Hearing Loss". National Institute on Deafness and Other Communication Disorders. October 2008.
- 1 2 Raphael, Y (2002). "Choclear pathology, sensory cell death and regeneration". Br. Med. Bull. 63: 25–38.
- ↑ Sun, H; Huang, A; Cao, S (2011). "Current status and prospects of gene therapy for the inner ear". Human gene therapy. 22 (11): 1311–22. doi:10.1089/hum.2010.246.
- ↑ Kawamoto, K; Ishimoto, S; Minoda, R (June 1, 2003). "Math1 gene transfer generates new cochlear hair cells in mature guinea pigs in vivo". J Neurosci. 23 (11): 4395–4400. PMID 12805278.
- ↑ Chisolm, TH; Johnson, CE; Danhauer, JL (2007). "A systematic review of health-related quality of life and hearing aids: final report of the American Academy of Audiology Task Force On the Health-Related Quality of Life Benefits of Amplification in Adults". J Am Acad Audiol. 18 (2): 151–183. doi:10.3766/jaaa.18.2.7.
- 1 2 "1.1 billion people at risk of hearing loss: WHO highlights serios threat posed by exposure to recreational noise". World Health Organization.
- 1 2 3 Rabinowitz, PM (2010). "Hearing loss and personal music players". BMJ (clinical research ed). 340: c1261. doi:10.1136/bmj.c1261.
- 1 2 Shargorodsky, J (2010). "Change in Prevalence of Hearing Loss in US Adolescents". JAMA. 304 (7): 722–778. doi:10.1001/jama.2010.1124.
- 1 2 3 "Hearing loss due to recreational exposure to loud sounds: a review" (PDF). World Health Organization. 2015.
- ↑ Basner, M; Babisch, W; Davis, A (2014). "Auditory and non-auditory effects of noise on health". The Lancet. 383: 1325–1332. doi:10.1016/s0140-6736(13)61613-x.
- ↑ Cone, BK; Wake, M; Tobin, S (2010). "Slight-mild sensorineural hearing loss in children: audiometric, clinical, and risk factor profiles". Ear Hear. 31 (2): 202–212. doi:10.1097/AUD.0b013e3181c62263. PMID 20054279.
External links
- Noise-Induced Hearing Loss from the National Institutes of Health
- How to Prevent Noise-Induced Hearing Loss from the American Academy of Family Physicians.
- Dangerous Decibels Includes general information and a "virtual exhibit" as well as resources for teachers.
- NIOSH Noise and Hearing Loss Prevention Topic Page
- NIOSH Power Tools Sound Pressure and Vibrations Database
- New York City construction noise control products and vendor guidance sheet
- Online Audiometric Test Calibrated test, up to 80 dBHL. Confirm your hearing loss and track how it evolves over time.
- An online audiometric test featuring equal loudness curves
- NIOSH Buy Quiet Topic Page
