Advanced airway management
Advanced airway management is the subset of airway management that involves high skill and invasiveness. It comprises various medical procedures performed to create an open airway (a path between a patient’s lungs and the outside world).
This is accomplished by clearing or preventing obstructions of airways, often referred to as choking, cause by the tongue, the airways them self, foreign bodies or materials from the body it self, such as blood or aspiration.
Unlike basic airway management such as head-tilt or jaw-thrust maneuver, advanced airway management relies on the use of medical equipment and special training. Invasive airway management can be performed "blind" or with visualization of the glottis e.g. by the use of a laryngoscope.
In roughly increasing order of invasiveness are the use of supraglottic devices such as oropharyngeal or nasopharyngeal airways, followed by infraglottic techniques such as tracheal intubation and finally surgical methods.
Advanced airway management is a primary consideration in cardiopulmonary resuscitation, anaesthesia, emergency medicine and intensive care medicine.
Removal of foreign objects
In advanced airway management foreign objects are either removed by suction or with e.g. a Magill forceps under inspection of the airway with a laryngoscope or bronchoscope. If removal is not possible surgical methods should be considered.
Supraglottic techniques
Supraglottic techniques includes the use of supraglottic tubes, such as oropharyngeal (OPA) and Nasopharyngeal airways (NPA), and supraglottic devises such as laryngeal masks. Common for all supraglottic devises are that they are introduced into the pharynx, ensuring the upper respiratory tract remains open, without passing through the glottis and thereby entering the trachea.
Nasopharyngeal airway
Nasopharyngeal airways is a soft rubber or plastic hollow tube that is passed through the nose into the posterior pharynx. Patients tolerate NPAs more easily than OPAs, so NPAs can be used when the use of an OPA is difficult, such as when the patient's jaw is clenched or the patient is semiconscious and cannot tolerate an OPA.[1] NPAs are generally not recommended if there is suspicion of a fracture to the base of the skull, due to the possibility of the tube entering the cranium.[2] However, the actual risks of this complication occurring compared to the risks of damage from hypoxia if an airway is not used are debatable.[2][3]
Oropharyngeal airway

Oropharyngeal airways are rigid plastic curved devices, which are inserted through the patients mouth. It prevents the patients tongue from covering the epiglottis and thereby obstructing the airway. An oropharyngeal airway should only be used in a deeply unresponsive patient because in a responsive patient they can cause vomiting and aspiration by stimulating the gag reflex.[4]
Supraglottic airway
Supraglottic airways (or extraglottic devices[5]) are a family of devices that are inserted through the mouth to sit on top of the larynx. Supraglottic airways are used in the majority of operations performed under general anaesthesia.[6] Compared to a cuffed tracheal tube (see below), they give less protection against aspiration but are easier to insert and cause less laryngeal trauma.[5]
The best-known example is the laryngeal mask airway or LMA™. A laryngeal mask airway is an airway placed into the mouth and set over the glottis and inflated.[7] Other variations include devices with oesophageal access ports, so that a separate tube can be inserted from the mouth to the stomach to decompress accumulated gases and drain liquid contents.[5] Some devices can have an endotracheal tube passed through them into the trachea.[5]
Infraglottic techniques
Tracheal intubation

Tracheal intubation, often simply referred to as intubation, is the placement of a flexible plastic or rubber tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction. The most widely used route is orotracheal, in which an endotracheal tube is passed through the mouth and vocal apparatus into the trachea. In a nasotracheal procedure, an endotracheal tube is passed through the nose and vocal apparatus into the trachea.
Alternatives to standard endotracheal tubes includes laryngeal tube and combitube.
Surgical methods
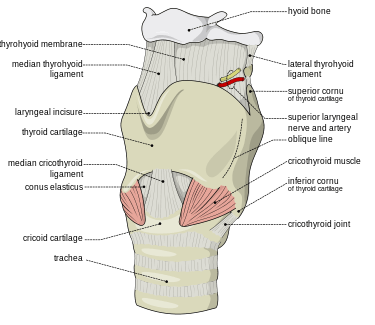
Surgical methods for airway management rely on making a surgical incision is made below the glottis in order to achieve direct access to the lower respiratory tract, bypassing the upper respiratory tract. Surgical airway management is often performed as a last resort in cases where orotracheal and nasotracheal intubation are impossible or contraindicated. Surgical airway management is also used when a person will need a mechanical ventilator for a longer period. Surgical methods for airway management include cricothyrotomy and tracheostomy.
A cricothyrotomy is an incision made through the skin and cricothyroid membrane to establish a patent airway during certain life-threatening situations, such as airway obstruction by a foreign body, angioedema, or massive facial trauma.[8] A cricothyrotomy is nearly always performed as a last resort in cases where orotracheal and nasotracheal intubation are impossible or contraindicated. Cricothyrotomy is easier and quicker to perform than tracheotomy, does not require manipulation of the cervical spine and is associated with fewer complications.[9]
A tracheotomy is a surgically created opening from the skin of the neck down to the trachea.[10] A tracheotomy may be considered where a person will need to be on a mechanical ventilator for a longer period.[10] The advantages of a tracheotomy include less risk of infection and damage to the trachea such as tracheal stenosis.[10]
Evaluation
Evaluation of airway management can be performed in several different ways by evaluation chest movement, loss of cyanosis, oxygen saturation or capnography.
See also
References
- ↑ Roberts K, Whalley H, Bleetman A (2005). "The nasopharyngeal airway: dispelling myths and establishing the facts". Emerg Med J. 22 (6): 394–6. doi:10.1136/emj.2004.021402. PMC 1726817
 . PMID 15911941.
. PMID 15911941. - 1 2 Ellis, D. Y. (2006). "Intracranial placement of nasopharyngeal airways: Is it all that rare?". Emergency Medicine Journal. 23 (8): 661–661. doi:10.1136/emj.2006.036541.
- ↑ Roberts, K.; Whalley, H.; Bleetman, A. (2005). "The nasopharyngeal airway: Dispelling myths and establishing the facts". Emergency Medicine Journal. 22 (6): 394–396. doi:10.1136/emj.2004.021402. PMC 1726817
 . PMID 15911941.
. PMID 15911941. - ↑ "Guedel airway". AnaesthesiaUK. 14 May 2010. Retrieved 23 May 2013.
- 1 2 3 4 Hernandez, MR; Klock, A; Ovassapian, A (2011). "Evolution of the Extraglottic Airway: A Review of Its History, Applications, and Practical Tips for Success". Anesthesia and Analgesia. 114 (2): 349–68. doi:10.1213/ANE.0b013e31823b6748. PMID 22178627.
- ↑ Cook, T; Howes, B. (2010). "Supraglottic airway devices: recent advances". Continuing Education in Anaesthesia, Critical Care and Pain. 11 (2): 56. doi:10.1093/bjaceaccp/mkq058.
- ↑ Davies PR, Tighe SQ, Greenslade GL, Evans GH (1990). "Laryngeal mask airway and tracheal tube insertion by unskilled personnel". The Lancet. 336 (8721): 977–979. doi:10.1016/0140-6736(90)92429-L. PMID 1978159. Retrieved 25 July 2010.
- ↑ Mohan, R; Iyer, R; Thaller, S (2009). "Airway management in patients with facial trauma". Journal of Craniofacial Surgery. 20 (1): 21–3. doi:10.1097/SCS.0b013e318190327a. PMID 19164982.
- ↑ Katos, MG; Goldenberg, D (2007). "Emergency cricothyrotomy". Operative Techniques in Otolaryngology. 18 (2): 110–4. doi:10.1016/j.otot.2007.05.002.
- 1 2 3 Gomes Silva, B. N.; Andriolo, R. G. B.; Saconato, H.; Atallah, Á. N.; Valente, O. (2012). Gomes Silva, Brenda Nazaré, ed. "Early versus late tracheostomy for critically ill patients". The Cochrane Library. doi:10.1002/14651858.CD007271.pub2.