Intestinal permeability
Intestinal permeability is a term describing the control of material passing from inside the gastrointestinal tract through the cells lining the gut wall, into the rest of the body. The intestine normally exhibits some permeability, which allows nutrients to pass through the gut, while also maintaining a barrier function to keep potentially harmful substances (such as antigens) from leaving the intestine and migrating to the body more widely.[1] In a healthy human intestine, small particles (< 4 Å in radius) can migrate through tight junction claudin pore pathways,[2] and particles up to 10-15 Å (3.5 kDa) can transit through the paracellular space uptake route.[3]
Physiology
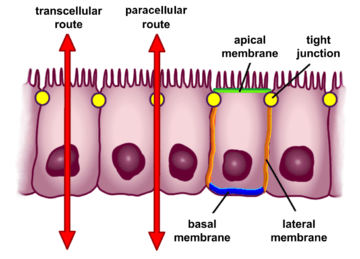
The barrier formed by the intestinal epithelium separates the external environment (the contents of the intestinal lumen) from the body[4] and is the most extensive and important mucosal surface of body.[5] The intestinal epithelium is composed of a single layer of cells and serves two crucial functions. First, it acts as a barrier, preventing the entry of harmful substances such as foreign antigens, toxins and microorganisms.[4][6] Second, it acts as a selective filter which facilitates the uptake of dietary nutrients, electrolytes, water and various other beneficial substances from the intestinal lumen.[4] Selective permeability is mediated via two major routes:[4]
- Transepithelial or transcellular permeability. This consists of specific transport of solutes across the epithelial cells. It is predominantly regulated by the activities of specialised transporters that translocate specific electrolytes, amino acids, sugars, short chain fatty acids and other molecules into or out of the cell.[4]
- Paracellular permeability. It depends on transport through the spaces that exist between epithelial cells. It is regulated by cellular junctions that are localized in the laminal membranes of the cells.[4] This is the main route of passive flow of water and solutes across the intestinal epithelium. Regulation depends on the intercellular tight junctions which have the most influence on paracellular transport.[7]
Modulation
One way in which intestinal permeability is modulated is via CXCR3 receptors in cells in the intestinal epithelium, which respond to zonulin.[8] Gliadin (a glycoprotein present in wheat) activates zonulin signaling irrespective of the genetic expression of autoimmunity, leading to increased intestinal permeability to macromolecules.[8][9] Bacterial pathogens such as cholera, select enteric viruses, and parasites modulate intestinal tight junction structure and function, and these effects may contribute to the development of chronic intestinal disorders.[8][10] Stress and infections also seem to cause perturbations in intestinal permeability.[9]
Clinical significance
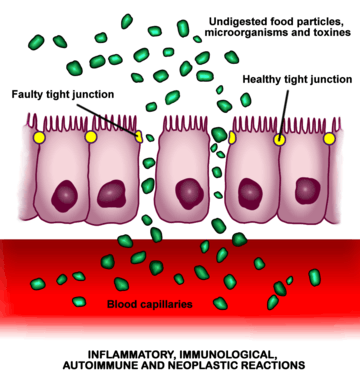
The opening of intercellular tight junctions (increased intestinal permeability) can allow passage of microbes, microbial products, and foreign antigens into the mucosa and the body proper. This can result in activation of the immune system and secretion of inflammatory mediators.[11]
Increased intestinal permeability is a factor in several diseases, such as Crohn's disease, celiac disease,[12] type 1 diabetes,[13] type 2 diabetes,[12] rheumatoid arthritis, spondyloarthropathies,[14] inflammatory bowel disease,[8][15] irritable bowel syndrome,[9] schizophrenia,[16][17] certain types of cancer,[8] obesity,[18] fatty liver,[19] atopy and allergic diseases,[13] among others. In the majority of cases, increased permeability develops prior to disease,[8] but the cause-effect relationship between increased intestinal permeability in most of these diseases is not clear.[15][20]
A well studied model is celiac disease, in which increased intestinal permeability appears secondary to the abnormal immune reaction induced by gluten and allows fragments of gliadin protein to get past the intestinal epithelium, triggering an immune response at the intestinal submucosa level that leads to diverse gastrointestinal or extra-gastrointestinal symptoms.[21][22] Other environmental triggers may contribute to alter permeability in celiac disease, as intestinal infections and iron deficiency.[21] Once established, this increase of permeability might self-sustain the inflammatory immune responses and perpetuate a vicious circle.[21] Eliminating gluten from the diet leads to normalization of intestinal permeability and the autoimmune process shuts off.[23]
Research directions
In normal physiology, glutamine plays a key role in signalling in enterocytes that are part of the intestinal barrier, but it is not clear if supplementing the diet with glutamine is helpful in conditions where there is increased intestinal permeability.[24]
Prebiotics and certain probiotics such as Escherichia coli Nissle 1917 have also been found to reduce increased intestinal permeability.[9]
Larazotide acetate (previously known as AT-1001) is a zonulin receptor antagonist that has been probed in clinical trials. It seems to be a drug candidate for use in conjunction with a gluten-free diet in people with celiac disease, with the aim to reduce the intestinal permeability caused by gluten and its passage through the epithelium, and therefore mitigating the resulting cascade of immune reactions.[22][25]
Leaky gut syndrome
A proposed medical condition called leaky gut syndrome has been popularized by some health practitioners, mainly of alternative medicine and nutritionists, which theorizes that restoring normal functioning of the gut wall can cure many systemic health conditions. There is little evidence to support this theory and that so-called 'treatments' for 'leaky gut syndrome', such as nutritional supplements (as those containing probiotics), herbal remedies, gluten-free foods, and low FODMAP, low sugar or antifungal diets, have any beneficial effect for most of the conditions they are claimed to help.[15]
See also
References
- ↑ M. Campieri; C. Fiocchi; S.B. Hanauer (31 March 2002). Inflammatory Bowel Disease: A Clinical Case Approach to Pathophysiology, Diagnosis, and Treatment. Springer. p. 7. ISBN 978-0-7923-8772-5.
- ↑ Thoma YM, Anderson JM, Turner JR (2012). Johnson LR, et al., eds. Tight Junctions and the Intestinal Barrier. Physiology of the Gastrointestinal Tract. 1. Academic Press. pp. 1043–. ISBN 978-0-12-382027-3.
- ↑ Fasano, A. (February 2012). "Leaky Gut and Autoimmune Diseases". Clinical Reviews in Allergy & Immunology (Review). 42 (1): 71–78. doi:10.1007/s12016-011-8291-x. PMID 22109896.
- 1 2 3 4 5 6 Groschwitz, Katherine R.; Hogan, Simon P. (2009-07-01). "Intestinal Barrier Function: Molecular Regulation and Disease Pathogenesis". The Journal of allergy and clinical immunology. 124 (1): 3–22. doi:10.1016/j.jaci.2009.05.038. ISSN 0091-6749. PMC 4266989
 . PMID 19560575.
. PMID 19560575. - ↑ Rao, Jaladanki N.; Wang, Jian-Ying (2010-01-01). "Intestinal Architecture and Development".
- ↑ Khan, Niamat; Asif, Abdul R. (2015-01-01). "Transcriptional Regulators of Claudins in Epithelial Tight Junctions". Mediators of Inflammation. 2015: 1–6. doi:10.1155/2015/219843. ISSN 0962-9351. PMC 4407569
 . PMID 25948882.
. PMID 25948882. - ↑ Näslund, Erik; Hellström, Per M. (2007-09-10). "Appetite signaling: from gut peptides and enteric nerves to brain". Physiology & Behavior. 92 (1-2): 256–262. doi:10.1016/j.physbeh.2007.05.017. ISSN 0031-9384. PMID 17582445.
- 1 2 3 4 5 6 Fasano A (Jan 2011). "Zonulin and its regulation of intestinal barrier function: the biological door to inflammation, autoimmunity, and cancer". Physiol Rev. (Review). 91 (1): 151–75. doi:10.1152/physrev.00003.2008. PMID 21248165.
- 1 2 3 4 Rapin JR, Wiernsperger N (2010). "Possible links between intestinal permeability and food processing: A potential therapeutic niche for glutamine". Clinics (Sao Paulo) (Review). 65 (6): 635–43. doi:10.1590/S1807-59322010000600012. PMC 2898551
 . PMID 20613941.
. PMID 20613941. - ↑ O'Hara, JR; Buret, AG (2008). "Mechanisms of intestinal tight junctional disruption during infection". Frontiers in Bioscience. 13: 7008–21. doi:10.2741/3206. PMID 18508712.
- ↑ Márquez, M; Fernández Gutiérrez, Del Álamo C; Girón-González, JA (2016). "Gut epithelial barrier dysfunction in human immunodeficiency virus-hepatitis C virus coinfected patients: Influence on innate and acquired immunity.". World J. Gastroenterol. 22: 1433–48. doi:10.3748/wjg.v22.i4.1433. PMC 4721978
 . PMID 26819512.
. PMID 26819512. - 1 2 Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M, Tilg H, Watson A, Wells JM (Nov 18, 2014). "Intestinal permeability--a new target for disease prevention and therapy". BMC Gastroenterol (Review). 14: 189. doi:10.1186/s12876-014-0189-7. PMC 4253991
 . PMID 25407511.
. PMID 25407511. - 1 2 Viggiano D, Ianiro G, Vanella G, Bibbò S, Bruno G, Simeone G, et al. (2015). "Gut barrier in health and disease: focus on childhood" (PDF). Eur Rev Med Pharmacol Sci. 19 (6): 1077–85. PMID 25855935.
- ↑ Yeoh N, Burton JP, Suppiah P, Reid G, Stebbings S (Mar 2013). "The role of the microbiome in rheumatic diseases". Curr Rheumatol Rep (Review). 15 (3): 314. doi:10.1007/s11926-012-0314-y. PMID 23378145.
- 1 2 3 "Leaky gut syndrome". NHS Choices. 26 February 2015. Retrieved 15 August 2016.
- ↑ Yarandi SS, Peterson DA, Treisman GJ, Moran TH, Pasricha PJ (2016). "Modulatory Effects of Gut Microbiota on the Central Nervous System: How Gut Could Play a Role in Neuropsychiatric Health and Diseases". J Neurogastroenterol Motil (Review). 22 (2): 201–12. doi:10.5056/jnm15146. PMC 4819858
 . PMID 27032544.
. PMID 27032544. In patients with schizophrenia, there are increased intestinal permeability and change in intestinal function
- ↑ Severance EG, Yolken RH, Eaton WW (2016). "Autoimmune diseases, gastrointestinal disorders and the microbiome in schizophrenia: more than a gut feeling". Schizophr Res (Review). 176 (1): 23–35. doi:10.1016/j.schres.2014.06.027. PMC 4294997
 . PMID 25034760.
. PMID 25034760. - ↑ Teixeira TF, Collado MC, Ferreira CL, Bressan J, Peluzio Mdo C (September 2012). "Potential mechanisms for the emerging link between obesity and increased intestinal permeability". Nutr Res (Review). 32 (9): 637–47. doi:10.1016/j.nutres.2012.07.003. PMID 23084636.
- ↑ Festi D, Schiumerini R, Eusebi LH, Marasco G, Taddia M, Colecchia A (November 2014). "Gut microbiota and metabolic syndrome". World J. Gastroenterol. (Review). 20 (43): 16079–16094. doi:10.3748/wjg.v20.i43.16079. PMC 4239493
 . PMID 25473159.
. PMID 25473159. - ↑ Kiefer, D; Ali-Akbarian, L (2004). "A brief evidence-based review of two gastrointestinal illnesses: Irritable bowel and leaky gut syndromes". Alternative Therapies in Health and Medicine. 10 (3): 22–30; quiz 31, 92. PMID 15154150.
- 1 2 3 Heyman M, et al. (Sep 2012). "Intestinal permeability in coeliac disease: insight into mechanisms and relevance to pathogenesis". Gut (Review). 61 (9): 1355–64. doi:10.1136/gutjnl-2011-300327. PMID 21890812.
Changes in intestinal paracellular and transcellular permeability appear secondary to the abnormal immune reaction induced by gluten. Gliadin was suggested to increase junction permeability to small molecules through the release of prehaptoglobin-2. Environmental triggers of CD other than gliadin may also promote changes in permeability. Intestinal infection and iron deficiency can stimulate the expression of the transferrin receptor (TfR) CD71 in enterocytes. ... Once established, the alterations in intestinal permeability, notably the retro-transport of IgA-gliadin peptides, might self-sustain the inflammatory immune responses and perpetuate a vicious circle.
- 1 2 Khaleghi, Shahryar; Ju, Josephine M.; Lamba, Abhinav; Murray, Joseph A. (Jan 2016). "The potential utility of tight junction regulation in celiac disease: focus on larazotide acetate". Therapeutic Advances in Gastroenterology (Review. Research Support, N.I.H., Extramural). 9 (1): 37–49. doi:10.1177/1756283X15616576. ISSN 1756-283X. PMC 4699279
 . PMID 26770266.
. PMID 26770266. - ↑ Fasano A (2012). "Intestinal permeability and its regulation by zonulin: diagnostic and therapeutic implications". Clin Gastroenterol Hepatol (Review). 10 (10): 1096–100. doi:10.1016/j.cgh.2012.08.012. PMC 3458511
 . PMID 22902773.
. PMID 22902773. - ↑ Akobeng, AK; Elawad, M; Gordon, M (8 February 2016). "Glutamine for induction of remission in Crohn's disease.". The Cochrane database of systematic reviews. 2: CD007348. PMID 26853855.
- ↑ Crespo Pérez L, et al. (Jan 2012). "Non-dietary therapeutic clinical trials in coeliac disease". Eur J Intern Med. (Review). 23 (1): 9–14. doi:10.1016/j.ejim.2011.08.030. PMID 22153524.