Immune cycle
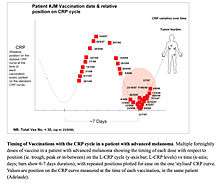
The immune cycle is a term that describes the natural homeostatic oscillation of the immune system when chronic inflammation is occurring.[1] Similar to the menstrual cycle, the exact periodicity (wavelength) and waveform of each particular individual patient is different.[1] That is, different people have different immune cycles although the cycle typically repeats itself approximately every 7-days on average.[1]

C-reactive protein levels in the blood need to be measured every few days in order to have enough time points to show a repeating fluctuation (a wave-like cycle).[1][2] This is caused by the synchronous division of T cells over time, with T-effector cells boosting immune activity followed by T-receptor cells suppressing the immune response.[2]
Although the exact reason for the immune cycle is not yet clear, it appears to be a result of repeating, alternating stimulation and inhibition of the immune response, which has been proved in cancer patients.[1] Many cycles occur in the body - like temperature regulation and hormone levels - and the exact cause for these cycles is also unknown, but it is thought to involve the hypothalamus.
Discovery

The idea of an immune cycle has existed for many years. In 1891, Dr William Coley noticed that some of his patients responded better to treatment than other patients, even with complete responses.[2] Almost a century later, in 1975, physicist George Irving Bell developed a mathematical equation to predict a hypothetical immune cycle. Dr Robert North, writing in the 1980s, demonstrated that chemotherapy encouraged the growth of tumors in mice, whose immune systems are very similar to humans.[3] Unfortunately, these pioneers were unable to prove its existence, particularly since the necessary technology had not yet come into existence.[2]
In the late 1990s, Associate Professor Brendon Coventry noticed that some of his patients responded better to a Melanoma vaccine than other patients despite receiving identical treatment.[4] When local cancer tumours where injected with the vaccine, cancers that had not been injected began to shrink as well, thus indicating an immunogenic relationship.[5] These observations led him to speculate that the immune system operates in a cyclical manner, with peaks and troughs.[2] Operating on this theory, Coventry was able to increase complete response rates to treatment of advanced melanoma from 7% to 17% and without noticeable negative side effects to chemotherapy and radiotherapy.[6][7]
In 2004, Associate Professor Manfred W. Beilharz et al. from the University of Western Australia began reporting on similar patterns in the treatment of HIV/AIDS infected mice.[8]
The 2009 publication of CRP identifies homeostatic immune oscillations in cancer patients: a potential treatment targeting tool? in the Journal of Translational Medicine, of which Coventry was the lead author, signalled the first time the immune cycle had been proven to exist in some form.[1] Coventry et al. charted the immune cycle in a process referred to as 'immune cycle mapping'.[1]
Developments
In 2010, Professor Michael Quinn from the Royal Melbourne Hospital announced that trials would be conducted on women suffering from ovarian cancer.[9] Dr Roxana S. Dronca et al. from the Mayo Clinic found that the immune cycle is also evident in fluctuations beyond C-reactive protein, as it can be seen in "infradian immune biorhythms of both immune cell subpopulations and cytokines."[10]
Cancer

According to a 2012 article in Cancer Management and Research, a well timed treatment and the use of agent Interleukin 2 can force the immune system into overdrive, expanding and maximising the period of T-effector cell activity.[1][11] According to Coventry, "[t]he immune system works in waves that seems to be switching on and off constantly. And now what we're trying to do is see whether we can identify periods or phases in that cycle where we could target [treatments] more effectively..."[6]
However, the research can also apply to Chemotherapy and Radiotherapy more generally, because it is applicable to the treatment of cancers that are, or are likely to be, immunogenic.[12] What this discovery shows is that a patient's treatment outcome may be largely determined by when treatment is administered in relation to their immune cycle, making treatment more a game of chance than a game with fixed rules.[13] Crucially, the ability to administer treatment at the most effective time in a patient's immune cycle means that significantly smaller dosages of chemotherapy can be used, which in turn means far fewer negative side effects to treatment.[2][14]
"Everything in nature exists in a delicate balance. The mammalian immune system has finely tuned opposing forces of immunity and tolerance. This balance can allow vigorous and selective responses to microorganisms and cancer while avoiding damaging responses to normal healthy tissue." Brendon Coventry et al., May 2010[2]
Public Awareness
The Australian Melanoma Research Foundation has undertaken many initiatives to promote this research and the potential benefits it could have on cancer patients, as well as advertising clinical trials.[15] Australian Senator Nick Xenophon has helped raise public awareness about this research, a fact that has been noted in the acknowledgements of numerous journal articles.[14]
Numerous submissions and presentations on these findings were made to committees of the Parliament of Australia. In a 2014 submission to the Standing Committee on Health into Skin Cancer in Australia, the Australian Melanoma Research Foundation stated that without the application of the new knowledge on the immune cycle cancer treatment was a "mathematically random" process.[16] It was also revealed that treatment on mice with the new knowledge resulted in a "complete eradication of established tumours in 60% of mice".[16] Their 2015 submission to the Senate Standing Committee on Community Affairs Inquiry into the Availability of new, innovative and specialist cancer drugs in Australia states that the 5 year survival rate of patients with advanced cancer is consistent with statistical probability that a patients treatment will be administered at exactly the right place in their immune cycle.[17]
In 2013, Dr Svetomir Markovic of the Mayo Clinic gave a public lecture in which he described the immune cycle and the potential developments to medicine it provides.[18]
Further reading
- Coventry BJ, Baum D, Lilly, "C Long-term survival in advanced melanoma patients using repeated therapies: successive immunomodulation improving the odds?" Cancer Management and Research, 2015, 7: 93–103.
- Coventry BJ, Lilly C, Hersey P, Michele A, Bright R "Prolonged Repeated Vaccine Immuno-Chemotherapy Induces Long-Term Clinical Responses and Survival for Advanced Metastatic Melanoma," Journal of Immunotherapy of Cancer 2014, 2: 9.
- Coventry BJ, Lilly C, "Table of Comparison of Reported Clinical Effectiveness of Treatments for Metastatic Melanoma," Australian Melanoma Research Foundation, 2014, www.melanomaresearch.com.au.
- Coventry BJ, Ashdown ML. "Complete clinical responses to cancer therapy caused by multiple divergent approaches: a repeating theme lost in translation," Cancer and Management Research, 2012, 4: 137-149.
- Coventry BJ, Ashdown ML. "The 20th anniversary of interleukin-2 therapy: bimodal role explaining longstanding random induction of complete clinical responses." Cancer and Management Research, 2012, 4: 215-21.
- Dronca RS, Leontovich AA, Nevala WK, and Markovic SN, "Personalized therapy for metastatic melanoma: could timing be everything?" Future Oncology, (2012), 8(11): 1401-1406
- Coventry BJ, Hersey P, Halligan A, Michele. "A Immuno-Chemotherapy Using Repeated Vaccine Treatment Can Produce Successful Clinical Responses in Advanced Metastatic Melanoma," Journal of Cancer Therapy, 2010, 1: 205-213.
- Coventry BJ, Ashdown ML, Quinn MA, Markovic SN, Yatomi-Clarke SL, Robinson AP, "CRP identifies homeostatic immune oscillations in cancer patients: potential treatment targeting tool?" Journal of Translational Medicine, 2009, 7: 102. Review.
References
- 1 2 3 4 5 6 7 8 Coventry, BJ; Ashdown, ML; Quinn, MA; Markovic, SN; Yatomi-Clarke, SL; Robinson, AP (30 November 2009). "CRP identifies homeostatic immune oscillations in cancer patients: a potential treatment targeting tool?". Journal of translational medicine. 7: 102. doi:10.1186/1479-5876-7-102. PMID 19948067.
- 1 2 3 4 5 6 7 "A Matter Of Time - Australasian Science Magazine". australasianscience.com.au.
- ↑ Ibid.
- ↑ http://www.theaustralian.com.au/national-affairs/budget-2015/budget-grants-regime-ignores-innovation-cancer-pioneer/story-fntfbo9p-1227358206121
- ↑ http://www.surgeons.org/media/21677517/ASC-Media-Release-Unexpected-Benefits-Observed-in-Cancer-Treatments.pdf
- 1 2 "AM - Melanoma vaccine increases survival rate 17/04/2014". abc.net.au.
- ↑ "Melanoma vaccine giving cancer victims hope". ABC News.
- ↑ Manfred W. Beilharz et al. “Timed Ablation of Regulatory CD4+ T Cells Can Prevent Murine AIDS Progression,” The Journal of Immunology 172 (2004)
- ↑ http://www.smh.com.au/lifestyle/diet-and-fitness/radical-ovarian-cancer-treatment-offers-hope-20100223-p0tf.html
- ↑ Dronca RS, Leontovich AA, Nevala WK, and Markovic SN, "Personalized therapy for metastatic melanoma: could timing be everything?" Future Oncology, (2012), 8(11): 1401-1406
- ↑ Brendon J. Coventry and Martin L. Ashdown, “Complete Clinical Responses to Cancer Therapy Caused by Multiple Divergent Approaches: A Repeating Theme Lost in Translation,” Cancer Management and Research (2012).
- ↑ New Zealand Herald. "Long-held breast cancer theories could be inaccurate". nzherald.co.nz.
- ↑ "Beat Cancer Project - Cancer Council SA". Cancer Council South Australia.
- 1 2 Brendon J. Coventry et al. “Prolonged Repeated Vaccine Immuno-Chemotherapy Induces Lomg-Term Clinical Responses and Survival for Advanced Metastatic Melanoma,” Journal for ImmunoTherapy of Cancer 2 (2014)
- ↑ Melanoma Research. "Australian Melanoma Research Foundation - Melanoma Vaccine Trial". melanomaresearch.com.au.
- 1 2 "Submissions". aph.gov.au.
- ↑ http://www.aph.gov.au/Parliamentary_Business/Committees/Senate/Community_Affairs/Cancer_Drugs/Submissions
- ↑ Treatment of Metastatic Melanoma: Could Timing Be Everything?. YouTube. 24 April 2013.