Hashimoto's thyroiditis
| Hashimoto's thyroiditis | |
|---|---|
| Synonyms | chronic lymphocytic thyroiditis, autoimmune thyroiditis, struma lymphomatosa |
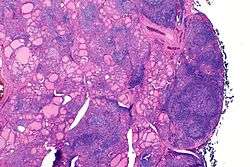 | |
| The thyroid of someone with Hashimoto's thyroiditis as seen with a microscope at low magnification | |
| Classification and external resources | |
| Specialty | endocrinology |
| ICD-10 | E06.3 |
| ICD-9-CM | 245.2 |
| OMIM | 140300 |
| DiseasesDB | 5649 |
| eMedicine | med/949 |
| Patient UK | Hashimoto's thyroiditis |
| MeSH | D050031 |
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, is an autoimmune disease in which the thyroid gland is gradually destroyed.[1] Early on there may be no symptoms.[1] Over time the thyroid may enlarge forming a painless goitre.[1] Some people eventually develop hypothyroidism with its accompanying weight gain, feeling tired, constipation, depression, and general pains.[1] After many years the thyroid typically shrinks in size.[1] Potential complications include thyroid lymphoma.[2]
Hashimoto's thyroiditis is thought to be due to a combination of genetic and environmental factors.[3] Risk factors include a family history of the condition and having another autoimmune diseases.[1] Diagnosis is confirmed with blood tests for TSH, T4, and antithyroid antibodies.[1] Other conditions that can produce similar symptoms include Graves’ disease and nontoxic nodular goiter.[4]
Hashimoto's thyroiditis, regardless of whether or not hypothyroidism is present, can be treated with levothyroxine.[1] If hypothyroidism is not present some may recommend no treatment while others may treat to try to reduce the size of the goitre.[1] Those affected should avoid eating large amounts of iodine; however, sufficient iodine is required especially during pregnancy.[1] Surgery is rarely required to treat the goitre.[4]
Hashimoto's thyroiditis affects about 5% of the population at some point in their life.[3] It typically begins between the ages of 30 and 50 and is much more common in women than men.[1][5] Rates of disease appear to be increasing.[4] It was first described by the Japanese physician Hakaru Hashimoto in 1912.[6] In 1957 it was recognized as an autoimmune disorder.[7]
Signs and symptoms
There are many symptoms that are attributed to Hashimoto's thyroiditis or Hashimoto's disease. The most common symptoms include the following: fatigue, weight gain, pale or puffy face, feeling cold, joint and muscle pain, constipation, dry and thinning hair, heavy menstrual flow or irregular periods, depression, panic disorder, a slowed heart rate, and problems getting pregnant and maintaining pregnancy.
Hashimoto’s disease is about seven times more common in women than in men. It can occur in teens and young women, but more commonly shows up in middle age, particularly for men. People who develop Hashimoto’s disease often have family members who have thyroid or other autoimmune diseases, and sometimes have other autoimmune diseases themselves.[8]
The thyroid gland may become firm, large, and lobulated in Hashimoto's thyroiditis, but changes in the thyroid can also be nonpalpable.[9] Enlargement of the thyroid is due to lymphocytic infiltration and fibrosis rather than tissue hypertrophy. Physiologically, antibodies against thyroid peroxidase (TPO) (also called TPOAb) and/or thyroglobulin cause gradual destruction of follicles in the thyroid gland. Accordingly, the disease can be detected clinically by looking for these antibodies in the blood. It is also characterized by invasion of the thyroid tissue by leukocytes, mainly T-lymphocytes. A rare but serious complication is thyroid lymphoma, generally the B-cell type, non-Hodgkin lymphoma.[10]
Risk factors
A family history of thyroid disorders is common, with the HLA-DR5 gene most strongly implicated conferring a relative risk of 3 in the UK. In addition Hashimoto's thyroiditis may be associated with CTLA-4 (Cytotoxic T-lymphocyte Antigen-4) gene polymorphisms that result in reduced functioning of the gene's products, which are associated with negative regulation of T-lymphocyte activity.[11] Downregulatory gene polymorphisms affecting CTLA4 are also associated with autoimmune pathology seen in development of type I diabetes.[12] The strong genetic component underscoring this theory is borne out in studies on monozygotic twins, with a concordance of 38-55%, with an even higher concordance of circulating thyroid antibodies not in relation to clinical presentation (up to 80% in monozygotic twins). Neither result was seen to a similar degree in dizygotic twins, offering strong favour for high genetic aetiology.[13]
Having another autoimmune diseases is a risk factor to develop Hashimoto’s thyroiditis, and the opposite is also true.[1] Autoimmune diseases most commonly associated to Hashimoto’s thyroiditis include celiac disease, type 1 diabetes, vitiligo and alopecia.[14]
Preventable environmental factors, including high iodine intake, selenium deficiency, as well as infectious diseases and certain drugs, have been implicated in the development of autoimmune thyroid disease in genetically predisposed individuals.[15] The genes implicated vary in different ethnic groups and the incidence is increased in people with chromosomal disorders, including Turner, Down, and Klinefelter syndromes usually associated with autoantibodies against thyroglobulin and thyroperoxidase. Progressive depletion of these cells as the cytotoxic immune response leads to higher degrees of primary hypothyroidism, presenting with a poverty of T3/T4 levels, and compensatory elevations of TSH.
Pathophysiology
There are multiple suggested mechanisms by which the pathology of Hashimoto's thyroiditis develops.
Various autoantibodies may be present against thyroid peroxidase, thyroglobulin and TSH receptors, although a small percentage of patients may have none of these antibodies present. As indicated in various twin studies a percentage of the population may also have these antibodies without developing Hashimoto's thyroiditis. Nevertheless, antibody-dependent cell-mediated cytotoxicity is a substantial factor behind the apoptotic fall-out of Hashimoto's thyroiditis. Activation of cytotoxic T-lymphocytes (CD8+ T-cells) in response to cell-mediated immune response affected by helper T-lymphocytes (CD4+ T-cells) is central to thyrocyte destruction. As is characteristic of type IV hypersensitivities, recruitment of macrophages is another effect of the helper T-lymphocyte activation, with Th1 axis lymphocytes producing inflammatory cytokines within thyroid tissue to further macrophage activation and migration into the thyroid gland for direct effect.
Gross morphological changes within the thyroid are seen in the general enlargement which is far more locally nodular and irregular than more diffuse patterns (such as that of hyperthyroidism). While the capsule is intact and the gland itself is still distinct from surrounding tissue, microscopic examination can provide a more revealing indication of the level of damage.[16]
Histologically, the hypersensitivity is seen as diffuse parenchymal infiltration by lymphocytes, particularly plasma B-cells, which can often be seen as secondary lymphoid follicles (germinal centers, not to be confused with the normally present colloid-filled follicles that constitute the thyroid). Atrophy of the colloid bodies is lined by Hürthle cells, cells with intensely eosinophilic, granular cytoplasm, a metaplasia from the normal cuboidal cells that constitute the lining of the thyroid follicles. Severe thyroid atrophy presents often with denser fibrotic bands of collagen that remains within the confines of the thyroid capsule.[17]
Diagnosis
Diagnosis is usually made by detecting elevated levels of anti-thyroid peroxidase antibodies (TPOAb) in the serum, but seronegative (without circulating autoantibodies) thyroiditis is also possible.[18]
Given the relatively non-specific symptoms of initial hypothyroidism, Hashimoto's thyroiditis is often misdiagnosed as depression, cyclothymia, PMS, chronic fatigue syndrome, fibromyalgia and, less frequently, as erectile dysfunction or an anxiety disorder. On gross examination, there is often presentation of a hard goitre that is not painful to the touch;[16] other symptoms seen with hypothyroidism, such as periorbital myxedema, depend on the current state of progression of the response, especially given the usually gradual development of clinically relevant hypothyroidism. Testing for thyroid-stimulating hormone (TSH), free T3, free T4, and the anti-thyroglobulin antibodies (anti-Tg), anti-thyroid peroxidase antibodies (anti-TPO, or TPOAb) and anti-microsomal antibodies can help obtain an accurate diagnosis.[19] Earlier assessment of the patient may present with elevated levels of thyroglobulin owing to transient thyrotoxicosis, as inflammation within the thyroid causes damage to the integrity of thyroid follicle storage of thyroglobulin; TSH is increased as the pituitary tries to increase production of T4 by the thyroid gland. This exposure of the body to substantial amounts of previously isolated thyroid enzymes is thought to contribute to the exacerbation of tolerance breakdown, giving rise to the more pronounced symptoms seen later in the disease. Lymphocytic infiltration of the thyrocyte-associated tissues often leads to the histologically significant finding of germinal center development within the thyroid gland.
Hashimoto's when presenting as mania is known as Prasad's syndrome after Ashok Prasad, the psychiatrist who first described it.[20]
Treatment
Managing hormone levels
Hypothyroidism caused by Hashimoto's thyroiditis is treated with thyroid hormone replacement agents such as levothyroxine, triiodothyronine or desiccated thyroid extract. A tablet taken once a day generally keeps the thyroid hormone levels normal. In most cases, the treatment needs to be taken for the rest of the patient's life. In the event that hypothyroidism is caused by Hashimoto's thyroiditis, it is recommended that the TSH levels be kept under 3.0.[21]
Prognosis
Overt, symptomatic thyroid dysfunction is the most common complication, with about 5% of patients with subclinical hypothyroidism and chronic autoimmune thyroiditis progressing to thyroid failure every year. Transient periods of thyrotoxicosis (over-activity of the thyroid) sometimes occur, and rarely the illness may progress to full hyperthyroid Graves' disease with active orbitopathy (bulging, inflamed eyes). Rare cases of fibrous autoimmune thyroiditis present with severe dyspnea (shortness of breath) and dysphagia (difficulty swallowing), resembling aggressive thyroid tumors - but such symptoms always improve with surgery or corticosteroid therapy. Primary thyroid B cell lymphoma affects fewer than one in a thousand patients, and it is more likely to affect those with long-standing autoimmune thyroiditis.[22]
Epidemiology
This disorder is believed to be the most common cause of primary hypothyroidism in North America; as a cause of non-endemic goiter, it is among the most common.[23] Hashimoto's thyroiditis affects about 5% of the population at some point in their life.[3] About 1 to 1.5 in 1000 people have this disease at any point in time.[23] It occurs between eight and fifteen times more often in women than in men. Though it may occur at any age, including in children, it is most often observed in women between 30 and 60 years of age.[22] It is more common in regions of high iodine dietary intake, and among people who are genetically susceptible.[22]
History
Also known as Hashimoto's disease, Hashimoto's thyroiditis is named after the Japanese physician Hakaru Hashimoto (1881−1934) of the medical school at Kyushu University,[24] who first described the symptoms of patients with struma lymphomatosa, an intense infiltration of lymphocytes within the thyroid, in 1912 in a German publication.[25] The report gave new insight into a condition (hypothyroidism) more commonly seen in areas of iodine deficiency that was occurring in the developed world, and without evident causation by dietary deficiency.
In 1957 it was recognized as an autoimmune disorder and was the first organ-specific one identified.[7]
Pregnancy
Pregnancy challenges thyroid function, putting additional pressure on the organ to function properly. In pregnant women who are positive for Hashimoto's thyroiditis, this challenge can lead the thyroid either to have decreased functionality or to fail entirely.[26] Pregnant mothers who are at a risk for Hashimoto's thyroiditis or who have been diagnosed as TPOAb-positive should be aware of the risks to themselves and their fetuses if the disease goes untreated. "Thyroid peroxidase antibodies (TPOAb) are detected in 10% of pregnant women," which presents risks to those pregnancies.[26] Risk factors are primarily indicated for women whose low thyroid function has not been stabilized by medication. These factors include: low birth weight, neonatal respiratory distress and fetal abnormalities (such as hydrocephalus and hypospadias), miscarriage, and preterm delivery.[26][27] When Hashimoto's thyroiditis is medicated through levothyroxine replacement, embryo implantation rate and pregnancy outcome are improved.[27] The 2012 study by Lepoutre et al. supports not only treating pregnant women who are TPOAb-positive throughout the entirety of their pregnancies, but their research also strongly recommends universal screening of thyroid levels for pregnant women.[26] They also recommend consistent cooperation between obstetricians and endocrinologists throughout the patient's pregnancy to ensure a positive outcome.[26] This conclusion is also supported by the research conducted in 2013 by Budenhofer, et al., as well as the 2013 study of Balucan, et al.[28][29] In March 2015, the Endocrine Society clearly stated that it does recommend screening in pregnant women who are considered high-risk for thyroid autoimmune disease.[30]
It is also recommended for undiagnosed women to be tested for thyroid peroxides antibodies if they have ever been pregnant (regardless of birth outcome). In their 2014 study, Carlé, et al. concluded, "…previous pregnancy plays a major role in development of autoimmune overt hypothyroidism in premenopausal women, and the number of previous pregnancies should be taken into account when evaluating the risk of hypothyroidism in a young women [sic]."[31] According to the research conducted by Carlé, et al., risk for thyroid dysfunction as well as for thyroid antibody production increases when at-risk or previously diagnosed mothers have more than one pregnancy.
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Hashimoto's Disease". NIDDK. May 2014. Retrieved 9 August 2016.
- ↑ Noureldine, SI; Tufano, RP (January 2015). "Association of Hashimoto's thyroiditis and thyroid cancer.". Current opinion in oncology. 27 (1): 21–5. PMID 25390557.
- 1 2 3 Pyzik, A; Grywalska, E; Matyjaszek-Matuszek, B; Roliński, J (2015). "Immune disorders in Hashimoto's thyroiditis: what do we know so far?". Journal of immunology research. 2015: 979167. PMID 26000316.
- 1 2 3 Akamizu, T; Amino, N; DeGroot, LJ; De Groot, LJ; Beck-Peccoz, P; Chrousos, G; Dungan, K; Grossman, A; Hershman, JM; Koch, C; McLachlan, R; New, M; Rebar, R; Singer, F; Vinik, A; Weickert, MO (2000). "Hashimoto's Thyroiditis". PMID 25905412.
- ↑ Hiromatsu, Y; Satoh, H; Amino, N (2013). "Hashimoto's thyroiditis: history and future outlook.". Hormones (Athens, Greece). 12 (1): 12–8. PMID 23624127.
- ↑ Shoenfeld, Yehuda; Cervera, Ricard; Gershwin, M. Eric (2010). Diagnostic Criteria in Autoimmune Diseases. Springer Science & Business Media. p. 216. ISBN 9781603272858.
- 1 2 Moore, Elaine A.; Wilkinson, Samantha (2009). The Promise of Low Dose Naltrexone Therapy: Potential Benefits in Cancer, Autoimmune, Neurological and Infectious Disorders. McFarland. p. 30. ISBN 9780786452583.
- ↑ "Hashimoto's disease fact sheet". Office on Women's Health, U.S. Department of Health and Human Services, womenshealth.gov (or girlshealth.gov). 16 July 2012. Retrieved 23 November 2014.
- ↑ Page 56 in: Staecker, Hinrich; Thomas R. Van De Water; Van de Water, Thomas R. (2006). Otolaryngology: basic science and clinical review. Stuttgart: Thieme. ISBN 0-86577-901-5.
- ↑ Dayan CM, Daniels GH (1996). "Chronic autoimmune thyroiditis". N Engl J Med. pp. 335:99–107. Retrieved 11 April 2014.
- ↑ Kavvoura, F. K.; Akamizu, T.; Awata, T.; Ban, Y.; Chistiakov, D. A.; Frydecka, I.; Ghaderi, A.; Gough, S. C.; Hiromatsu, Y. (2007). "Cytotoxic T-Lymphocyte Associated Antigen 4 Gene Polymorphisms and Autoimmune Thyroid Disease: A Meta-Analysis". Journal of Clinical Endocrinology & Metabolism. 92 (8): 3162–70. doi:10.1210/jc.2007-0147. PMID 17504905.
- ↑ Jacobson, Eric M.; Tomer, Yaron (2007). "The CD40, CTLA-4, thyroglobulin, TSH receptor, and PTPN22 gene quintet and its contribution to thyroid autoimmunity: Back to the future". Journal of Autoimmunity. 28 (2–3): 85–98. doi:10.1016/j.jaut.2007.02.006. PMC 2043086
 . PMID 17369021.
. PMID 17369021. - ↑ Chistiakov, Dimitry A (2005). "Immunogenetics of Hashimoto's thyroiditis". Journal of Autoimmune Diseases. 2 (1): 1. doi:10.1186/1740-2557-2-1. PMC 555850
 . PMID 15762980.
. PMID 15762980. - ↑ Radetti G (2014). "Clinical aspects of Hashimoto's thyroiditis.". Endocr Dev (Review). 26: 158–70. doi:10.1159/000363162. PMID 25231451.
- ↑ Saranac, L.; Zivanovic, S.; Bjelakovic, B.; Stamenkovic, H.; Novak, M.; Kamenov, B. (2011). "Why is the Thyroid So Prone to Autoimmune Disease". Hormone Research in Paediatrics. 75 (3): 157–65. doi:10.1159/000324442. PMID 21346360.
- 1 2 Kumar, Vinay (2010). "24: The Endocrine System". Robbins and Cotran Pathologic Mechanisms of Disease (8th ed.). Philadelphia, PA: Elsevier. p. 1113.
- ↑ Kumar, Vinay (2010). "24: The Endocrine System". Robbins and Cotran Pathologic Mechanisms of Disease (8th ed.). Philadelphia, PA: Elsevier. pp. 1112–1113.
- ↑ Grani, Giorgio; Carbotta, Giovanni; Nesca, Angela; D’Alessandri, Mimma; Vitale, Martina; Del Sordo, Marianna; Fumarola, Angela (4 October 2014). "A comprehensive score to diagnose Hashimoto's thyroiditis: a proposal". Endocrine. doi:10.1007/s12020-014-0441-5.
- ↑ Giannini, AJ (1986). The Biological Foundations of Clinical Psychiatry. New Hyde Park, NY: Medical Examination Publishing Company. pp. 193–198. ISBN 0-87488-449-7.
- ↑ "Prasad's syndrome" (PDF).
- ↑ "Does Your Doctor Know About the New TSH Lab Standards?".
- 1 2 3 Fabrizio Monaco (2012). Thyroid Diseases. Taylor and Francis. p. 78. ISBN 9781439868393.
- 1 2 Kumar, Vinay (2010). "24: The Endocrine System". Robbins and Cotran Pathologic Mechanisms of Disease (8th ed.). Philadelphia, PA: Elsevier. pp. 1111–205.
- ↑ Hakaru Hashimoto at Who Named It?
- ↑ Hashimoto, H. (1912). "Zur Kenntnis der lymphomatösen Veränderung der Schilddrüse (Struma lymphomatosa)". Archiv für Klinische Chirurgie (in German). Berlin. 97: 219–248.
- 1 2 3 4 5 Lepoutre, Thibault; Debiève, Frederic; Gruson, Damien; Daumerie, Chantal (2012-01-01). "Reduction of Miscarriages through Universal Screening and Treatment of Thyroid Autoimmune Diseases". Gynecologic and Obstetric Investigation. 74 (4): 265–273. doi:10.1159/000343759.
- 1 2 Zaletel, Katja (2011). "Thyroid physiology and autoimmunity in pregnancy and after delivery". Expert review of clinical immunology. 7: 697–707. doi:10.1586/eci.11.42. Retrieved 4 October 2015.
- ↑ Budenhofer, Brigitte K.; Ditsch, Nina; Jeschke, Udo; Gärtner, Roland; Toth, Bettina (2012-10-27). "Thyroid (dys-)function in normal and disturbed pregnancy". Archives of Gynecology and Obstetrics. 287 (1): 1–7. doi:10.1007/s00404-012-2592-z. ISSN 0932-0067.
- ↑ Balucan, Francis S.; Morshed, Syed A.; Davies, Terry F. (2013-01-01). "Thyroid Autoantibodies in Pregnancy: Their Role, Regulation and Clinical Relevance". Journal of Thyroid Research. 2013: 1–15. doi:10.1155/2013/182472. PMC 3652173
 . PMID 23691429.
. PMID 23691429. - ↑ "Endocrine Experts Support Screening for Thyroid Dysfunction in Pregnant Women". Endocrine Society. Endocrine Society. 26 March 2015. Retrieved 4 October 2015.
- ↑ Carlé, Allan; Pedersen, Inge Bülow; Knudsen, Nils; Perrild, Hans; Ovesen, Lars; Rasmussen, Lone Banke; Laurberg, Peter (2014-04-02). "Development of Autoimmune Overt Hypothyroidism Is Highly Associated With Live Births and Induced Abortions but Only in Premenopausal Women". The Journal of Clinical Endocrinology & Metabolism. 99 (6): 2241–2249. doi:10.1210/jc.2013-4474. ISSN 0021-972X.
External links
- Hashimoto's disease at the Mayo Clinic
- Hall, Richard C.W.; Popkin, Michael K.; Devaul, Richard; Hall, Anne K.; Gardner, Earl R.; Beresford, Thomas P. (April 1986). "Psychiatric manifestations of Hashimoto's thyroiditis" (PDF). Psychosomatics. 23 (4): 337–42. doi:10.1016/S0033-3182(82)73397-3. PMID 6896238.