Gestational pemphigoid
| Gestational pemphigoid | |
|---|---|
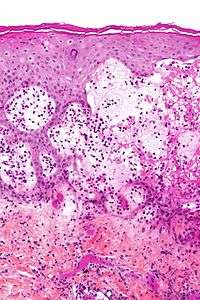 | |
| Micrograph of gestational pemphigiod showing the characteristic subepidermal blisters and abundant eosinophils. HPS stain. | |
| Classification and external resources | |
| Specialty | obstetrics |
| ICD-10 | O26.4 |
| ICD-9-CM | 646.8 |
| eMedicine | derm/178 |
| MeSH | D006559 |
Gestational pemphigoid or pemphigoid gestationis (PG) is a dermatosis of pregnancy,[1][2] being an autoimmune[3] blistering skin disease that occurs during pregnancy, typically in the second or third trimester, and/or immediately following pregnancy. It was originally called herpes gestationis because of the blistering appearance, although it is not associated with the herpes virus.
Presentation
Diagnosis of PG becomes clear when skin lesions progress to tense blisters during the second or third trimester. The face and mucous membranes are usually spared. PG typically starts as a blistering rash in the navel area and then spreads over the entire body. It is sometimes accompanied by raised, hot, painful welts called plaques. After one to two weeks, large, tense blisters typically develop on the red plaques, containing clear or blood-stained fluid.[4] PG creates a histamine response that causes extreme relentless itching (pruritus). PG is characterized by flaring and remission during the gestational and sometimes post partum period. Usually after delivery, lesions will heal within months, but may reoccur during menstruation.
Causes
Pathogenically, it is a Type II Hypersensitivity reaction where circulating complement-fixing IgG antibodies bind to an antigen (a 180-kDa protein, BP-180) in the hemidesmosomes (attach basal cells of epidermis to the basal lamina and hence to dermis) of the dermoepidermal junction (DEJ) , leading to blister formation as loss of hemidesmosomes causes the epidermis to separate from dermis. The immune response is even more highly restricted to the NC16A domain. The primary site of autoimmunity seems not to be the skin, but the placenta, as antibodies bind not only to the basement membrane zone of the epidermis, but also to that of chorionic and amniotic epitheli. Aberrant expression of MHC class II molecules on the chorionic villi suggests an allogenic immune reaction to a placental matrix antigen, thought to be of paternal origin .Recently, both IgA22 and IgE24 antibodies to either BP180 or BP230 have also been detected in pemphigoid gestationis.
Differential diagnosis
PG often is confused with pruritic urticarial papules and plaques of pregnancy (PUPPP), especially if it occurs in a first pregnancy. PUPPP typically begins in stretch mark areas of the abdomen and usually ends within two weeks after delivery. PUPPP is not an autoimmune disease.
Diagnosing PG is done by biopsy using direct immunofluorescence, appearance, and blood studies.[5]
Treatment
The most accepted way to treat PG is with the use of corticosteroids,[6] i.e. prednisone; and/or topical steroids, i.e. clobetasol and betamethasone. Suppressing the immune system with corticosteroids helps by decreasing the number of antibodies attacking the skin. Treating PG can be difficult and can take several months. Some cases of PG persist for many years. In the post partum period, if necessary, the full range of immunosuppressive treatment may be administered for cases unresponsive to corticosteroid treatments, such as tetracyclines, nicotinamide, cyclophosphamide, ciclosporin, goserelin, azathioprine, dapsone, rituximumab, or plasmaphoresis, or intravenous immunoglobulin may sometimes be considered when the symptoms are severe.
There is no cure for PG. Women who have PG are considered in remission if they are no longer blistering. Remission can last indefinitely, or until a subsequent pregnancy. PG usually occurs in subsequent pregnancies; however, it often seems more manageable because it is anticipated.
Support
Gestational pemphigoid can be a frightening and devastating condition. Because of its rarity, few studies have been conducted; the largest group studied included 87 women.[7]
Both a Facebook group ( https://www.facebook.com/groups/PemGest/) and a Yahoo group (https://groups.yahoo.com/neo/groups/PemGest/info) have been set up to help women and their families support each other and understand more about this disease and the impact it can have on mothers and their families.
Risk
Pregnant women with PG should be monitored for conditions that may affect the fetus, including, but not limited to, low or decreasing volume of amniotic fluid, preterm labor, and intrauterine growth retardation. Onset of PG in the first or second trimester and presence of blisters may lead to adverse pregnancy outcomes including decreased gestational age at delivery, preterm birth, and low birth weight children. Such pregnancies should be considered high risk and appropriate obstetric care should be provided. Systemic corticosteroid treatment, in contrast, does not substantially affect pregnancy outcomes, and its use for PG in pregnant women is justified.[8] PG typically reoccurs in subsequent pregnancies. Passive transfer of the mother’s antibodies to the fetus causes some (about 10%) newborns to develop mild skin lesions, but these typically will resolve within weeks of parturition.
See also
- Bullous pemphigoid
- Cicatricial pemphigoid
- List of target antigens in pemphigoid
- List of immunofluorescence findings for autoimmune bullous conditions
References
- ↑ Ambros-Rudolph CM, Müllegger RR, Vaughan-Jones SA, Kerl H, Black MM (March 2006). "The specific dermatoses of pregnancy revisited and reclassified: results of a retrospective two-center study on 505 pregnant patients". J. Am. Acad. Dermatol. 54 (3): 395–404. doi:10.1016/j.jaad.2005.12.012. PMID 16488288.
- ↑ Kroumpouzos G, Cohen LM (July 2001). "Dermatoses of pregnancy". J. Am. Acad. Dermatol. 45 (1): 1–19; quiz 19–22. doi:10.1067/mjd.2001.114595. PMID 11423829.
- ↑ Boulinguez S, Bédane C, Prost C, Bernard P, Labbé L, Bonnetblanc JM (2003). "Chronic pemphigoid gestationis: comparative clinical and immunopathological study of 10 patients". Dermatology (Basel). 206 (2): 113–9. doi:10.1159/000068467. PMID 12592077.
- ↑ Beard, M. P.; Millington, G. W. M (2012). "Recent developments in the specific dermatoses of pregnancy". Clinical and Experimental Dermatology. 37 (1): 1–5. doi:10.1111/j.1365-2230.2011.04173.x. PMID 22007708.
- ↑ BP180NC16a ELISA May Be Useful in Serodiagnosis of Pemphigoid Gestationis. Medscape: June 21, 2005
- ↑ Castro LA, Lundell RB, Krause PK, Gibson LE (November 2006). "Clinical experience in pemphigoid gestationis: report of 10 cases". J. Am. Acad. Dermatol. 55 (5): 823–8. doi:10.1016/j.jaad.2006.07.015. PMID 17052488.
- ↑ Jenkins RE, Hern S, Black MM (July 1999). "Clinical features and management of 87 patients with pemphigoid gestationis". Clin. Exp. Dermatol. 24 (4): 255–9. doi:10.1046/j.1365-2230.1999.00472.x. PMID 10457123.
- ↑ Chi, C-C.; Wang, S-H; Charles-Holmes, R.; Ambros-Rudolph, C.; Powell, J.; Jenkins, R.; Black, M.; Wojnarowska, F. (2012). "Pemphigoid gestationis: early onset and blister formation are associated with adverse pregnancy outcomes". British Journal of Dermatology. 160 (6): 1222–1228. doi:10.1111/j.1365-2133.2009.09086.x. PMID 19298272.