Dental radiography
| Dental radiography | |
|---|---|
| Intervention | |
| ICD-9-CM | 87.0-87.1 |
Dental Radiographs are commonly called x-rays. Dentists use radiographs for many reasons: to find hidden dental structures, malignant or benign masses, bone loss, and cavities.
A radiographic image is formed by a controlled burst of X-ray radiation which penetrates oral structures at different levels, depending on varying anatomical densities, before striking the film or sensor. Teeth appear lighter because less radiation penetrates them to reach the film. Dental caries, infections and other changes in the bone density, and the periodontal ligament, appear darker because X-rays readily penetrate these less dense structures. Dental restorations (fillings, crowns) may appear lighter or darker, depending on the density of the material.
The dosage of X-ray radiation received by a dental patient is typically small (around 0.150 mSv for a full mouth series, according to the American Dental Association website), equivalent to a few days' worth of background environmental radiation exposure, or similar to the dose received during a cross-country airplane flight (concentrated into one short burst aimed at a small area). Incidental exposure is further reduced by the use of a lead shield, lead apron, sometimes with a lead thyroid collar. Technician exposure is reduced by stepping out of the room, or behind adequate shielding material, when the X-ray source is activated.
Once photographic film has been exposed to X-ray radiation, it needs to be developed, traditionally using a process where the film is exposed to a series of chemicals in a dark room, as the films are sensitive to normal light. This can be a time-consuming process, and incorrect exposures or mistakes in the development process can necessitate retakes, exposing the patient to additional radiation. Digital x-rays, which replace the film with an electronic sensor, address some of these issues, and are becoming widely used in dentistry as the technology evolves. They may require less radiation and are processed much more quickly than conventional radiographic films, often instantly viewable on a computer. However digital sensors are extremely costly and have historically had poor resolution, though this is much improved in modern sensors.
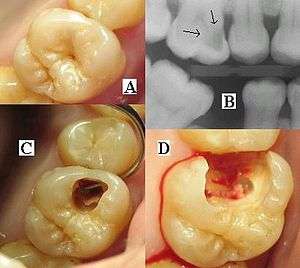
It is possible for both tooth decay and periodontal disease to be missed during a clinical exam, and radiographic evaluation of the dental and periodontal tissues is a critical segment of the comprehensive oral examination. The photographic montage at right depicts a situation in which extensive decay had been overlooked by a number of dentists prior to radiographic evaluation
Intraoral radiographic views
Placing the radiographic film or sensor inside the mouth produces an intraoral radiographic view.
Periapical view
The periapical(PA) view is taken of both anterior and posterior teeth. The objective of this type of view is to capture the tip of the root on the film. This is often helpful in determining the cause of pain in a specific tooth, because it allows a dentist to visualize the tooth as well as the surrounding bone in their entirety. This view is often used to determine the need for endodontic therapy as well as to visualize the successful progression of endodontic therapy once it is initiated. It can be used in case of detection hyperdontia (supernumerary teeth) & impacted teeth.
The name periapical is derived from the Greek peri, which means "around," and apical, which means "tip."
Bitewing view
The bitewing view is taken to visualize the crowns of the posterior teeth and the height of the alveolar bone in relation to the cementoenamel junctions, which are the demarcation lines on the teeth which separate tooth crown from tooth root. Routine bitewing radiographs are commonly used to examine for interdental caries and recurrent caries under existing restorations. When there is extensive bone loss, the films may be situated with their longer dimension in the vertical axis so as to better visualize their levels in relation to the teeth. Because bitewing views are taken from a more or less perpendicular angle to the buccal surface of the teeth, they more accurately exhibit the bone levels than do periapical views. Bitewings of the anterior teeth are not routinely taken. The name bitewing refers to a little tab of paper or plastic situated in the center of the X-ray film, which when bitten on, allows the film to hover so that it captures an even amount of maxillary and mandibular information.
Occlusal view
The occlusal view reveals the skeletal or pathologic anatomy of either the floor of the mouth or the palate. The occlusal film, which is about three to four times the size of the film used to take a periapical or bitewing, is inserted into the mouth so as to entirely separate the maxillary and mandibular teeth, and the film is exposed either from under the chin or angled down from the top of the nose. Sometimes, it is placed in the inside of the cheek to confirm the presence of a sialolith in Stenson's duct, which carries saliva from the parotid gland. The occlusal view is not included in the standard full mouth series.
Full Mouth Series
A full mouth series is a complete set of intraoral X-rays taken of a patients' teeth and adjacent hard tissue.[1] This is often abbreviated as either FMS or FMX (or CMRS, meaning Complete Mouth Radiographic Series). The full mouth series is composed of 18 films, taken the same day:
- four bitewings
- eight posterior periapicals
- two maxillary molar periapicals (left and right)
- two maxillary premolar periapicals (left and right)
- two mandibular molar periapicals (left and right)
- two mandibular premolar periapicals (left and right)
- six anterior periapicals
- two maxillary canine-lateral incisor periapicals (left and right)
- two mandibular canine-lateral incisor periapicals (left and right)
- two central incisor periapicals (maxillary and mandibular)
The Faculty of General Dental Practice of the Royal College of Surgeons of England publication Selection Criteria in Dental Radiography holds that given current evidence full mouth series are to be discouraged due to the large numbers of radiographs involved, many of which will not be necessary for the patient's treatment. An alternative approach using bitewing screening with selected periapical views is suggested as a method of minimising radiation dose to the patient while maximizing diagnostic yield.
Extraoral radiographic views
Placing the photographic film or sensor outside the mouth, on the opposite side of the head from the X-ray source, produces an extra-oral radiographic view.
A lateral cephalogram is used to evaluate dentofacial proportions and clarify the anatomic basis for a malocclusion, and an antero-posterior radiograph provides a face-forward view.
Panoramic films

Panoramic films are extraoral films, in which the film is exposed while outside the patient's mouth, and they were developed by the United States Army as a quick way to get an overall view of a soldier's oral health. Exposing eighteen films per soldier was very time consuming, and it was felt that a single panoramic film could speed up the process of examining and assessing the dental health of the soldiers; as soldiers with toothache were incapacitated from duty. It was later discovered that while panoramic films can prove very useful in detecting and localizing mandibular fractures and other pathologic entities of the mandible, they were not very good at assessing periodontal bone loss or tooth decay.[2]
Computed tomography
There is increasing use of CT (computed tomography) scans in dentistry, particularly to plan dental implants; there may be significant levels of radiation and potential risk. Specially designed CBCT (cone beam CT) scanners can be used instead, which produce adequate imaging with a stated tenfold reduction in radiation.[3] Controversy surrounds the degree of radiation reduction though as the highest quality cone beam scans use radiation doses not dissimilar to modern conventional CT scans.[4]
See also
- Orthopantomogram
- X-ray
- Radiography
- Digital radiography
- Allan G. Farman – Oral and Maxillofacial Radiologist and Professor
- Vijay P. Parashar – Oral and Maxillofacial Radiologist and Associate Professor
References
- ↑ Carranza's Clinical Periodontology, 9th Ed., W.B. Saunders 2002, page 435.
- ↑ Carranza's Clinical Periodontology, 9th Ed., W.B. Saunders 2002, page 436.
- ↑ Dr. Bernard Friedland, Harvard School of Dental Medicine, 1dec07
- ↑ Dory, Miri (August 12, 2014). "Digital Dental Imaging in the Cloud", Cephx.
External links
- Frequently Asked Questions about X-Rays - American Dental Association.
- Discussions on Digital Radiography in Dentistry DDSGadget