Chlamydia trachomatis
| Chlamydia trachomatis | |
|---|---|
 | |
| Chlamydia trachomatis in brown | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Chlamydiae |
| Class: | Chlamydiae |
| Order: | Chlamydiales |
| Family: | Chlamydiaceae |
| Genus: | Chlamydia |
| Species: | C. trachomatis |
| Binomial name | |
| Chlamydia trachomatis[1] (Busacca 1935) Rake 1957 emend. Everett et al. 1999 | |
| Synonyms | |
| |
Chlamydia trachomatis (/kləˌmɪdiə/ /trəˈkoʊmətᵻs/), commonly known as chlamydia,[2] is one of four bacterial species in the genus Chlamydia.[3] Chlamydia is a genus of pathogenic bacteria that are obligate intracellular parasites. C. trachomatis is a Gram-negative bacterium. It is ovoid in shape and nonmotile. The bacteria are nonspore-forming, but the elementary bodies act like spores when released into the host.[4] The inclusion bodies of C. trachomatis were first described in 1942. C. trachomatis agent was first cultured in the yolk sacs of eggs by Professor Tang Fei-fan, et al. in 1957.[5][6]
Disorders caused by C. trachomatis include chlamydia, trachoma, lymphogranuloma venereum, nongonococcal urethritis, cervicitis, salpingitis, pelvic inflammatory disease, and pneumonia.
C. trachomatis includes three human biovars:
- Serovars Ab, B, Ba, or C — cause trachoma: infection of the eyes, which can lead to blindness
- Serovars D-K — cause urethritis, pelvic inflammatory disease, ectopic pregnancy, neonatal pneumonia, and neonatal conjunctivitis
- Serovars L1, L2, and L3 — lymphogranuloma venereum[7]
Many C. trachomatis strains have an extrachromosomal plasmid.[8]
Chlamydia species can exchange DNA between the different strains, thus the evolution of new strains is common.[9]
Identification
Chlamydia species are readily identified and distinguished from other Chlamydia species using DNA-based tests.
Most strains of C. trachomatis are recognized by monoclonal antibodies (mAbs) to epitopes in the VS4 region of MOMP.[10] However, these mAbs may also cross-react with two other Chlamydia species, C. suis and C. muridarum.
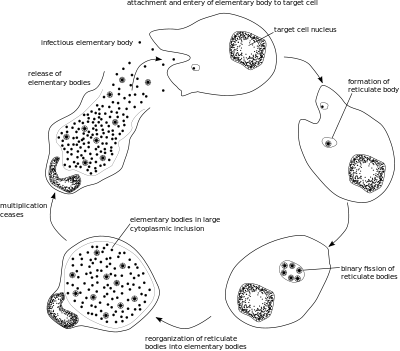
Lifecycle
Clinical significance
Clinical signs and symptoms of C. trachomatis infection and gonorrhea infection are indistinguishable.[11] Both are common causes of urethritis.[7] C. trachomatis is the single most important infectious agent associated with blindness (trachoma); about 84 million worldwide suffer C. trachomatis eye infections and 8 million are blinded as a result of the infection.[12]
Presentation
Most people infected with C. trachomatis are asymptomatic. However, the bacteria can present in one of three ways: genitourinary, pulmonary, and ocular. Genitourinary cases can include genital discharge, vaginal bleeding or pruritus, and dysuria.[13]
Prevalence
Three times as many women as men are diagnosed with genitourinary C. trachomatis infections. Women aged 15–19 have the highest prevalence, followed by women aged 20–24, although the rate of increase of diagnosis is greater for men than for women. Risk factors for genitourinary infections include unprotected sex with multiple partners, lack of condom use, and living in an urban area.
Pulmonary infections can occur in infants born to women with active chlamydia infections, although the rate of infection is less than 10%.[13]
Ocular infections take the form of conjunctivitis or trachoma, both in adults and children. Trachoma is the primary source of infectious blindness in some parts of rural Africa and Asia[14] and is a neglected tropical disease that has been targeted by the World Health Organization for elimination by 2020.
Treatment
Treatment depends on the infection site, age of the patient, and whether another infection is present. Having a C. trachomatis and one or more other sexually transmitted infections at the same time is possible. Treatment is often done with both partners simultaneously to prevent reinfection. C. trachomatis may be treated with several antibiotic medications, including azithromycin, erythromycin, or ofloxacin.[11]
If treatment is necessary during pregnancy, levofloxacin, ofloxacin, and doxycycline are not prescribed. In the case of a patient who is pregnant, the medications typically prescribed are azithromycin, amoxicillin, and erythromycin. Amoxicillin has fewer side effects than the other medications for treating antenatal C. trachomatis infection. Retesting during pregnancy can be performed three weeks after treatment. If the risk of reinfection is high, screening can be repeated throughout pregnancy.[11]
If the infection has progressed, ascending the reproductive tract and pelvic inflammatory disease develops, damage to the fallopian tubes may have already occurred. In most cases, the C. trachomatis infection is then treated on an outpatient basis with azithromycin or doxycycline. Treating the mother of an infant with C. trachomatis of the eye, which can evolve into a pneumonia, is recommended.[11]
Laboratory tests
- Nucleic acid amplification tests (NAATs) tests find the genetic material (DNA) of Chlamydia bacteria. These tests are the most sensitive tests available, meaning they are very accurate and are very unlikely to have false-negative test results. A polymerase chain reaction (PCR) test is an example of a nucleic acid amplification test. This test can also be done on a urine sample.
- Nucleic acid hybridization tests (DNA probe test) also find Chlamydia DNA. A probe test is very accurate, but is not as sensitive as NAATs.
- Enzyme-linked immunosorbent assay (ELISA, EIA) finds substances (Chlamydia antigens) that trigger the immune system to fight Chlamydia infection.
- Direct fluorescent antibody test also finds Chlamydia antigens.
- Chlamydia cell culture is a test in which the suspected Chlamydia sample is grown in a vial of cells. The pathogen infects the cells, and after a set incubation time (48 hours), the vials are stained and viewed on a fluorescent light microscope. Cell culture is more expensive and takes longer (two days) than the other tests. The culture must be grown in a laboratory.[15]
See also
References
- ↑ J.P. Euzéby. "Chlamydia". List of Prokaryotic names with Standing in Nomenclature. Retrieved 2008-09-11.
- ↑ "Chlamydia trachomatis".
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 463–70. ISBN 0-8385-8529-9.
- ↑ "Chlamydia - CDC Fact Sheet". Centers for Disease Control and Prevention (CDC).
- ↑ Darougar S, Jones BR, Kinnison JR, Vaughan-Jackson JD, Dunlop EM (December 1972). "Chlamydial infection. Advances in the diagnostic isolation of Chlamydia, including TRIC agent, from the eye, genital tract, and rectum". Br J Vener Dis. 48 (6): 416–20. doi:10.1136/sti.48.6.416. PMC 1048360
 . PMID 4651177.
. PMID 4651177. - ↑ Tang FF, Huang YT, Chang HL, Wong KC (1958). "Further studies on the isolation of the trachoma virus". Acta Virol. 2 (3): 164–70. PMID 13594716.
Tang FF, Chang HL, Huang YT, Wang KC (June 1957). "Studies on the etiology of trachoma with special reference to isolation of the virus in chick embryo". Chin Med J. 75 (6): 429–47. PMID 13461224.
Tang FF, Huang YT, Chang HL, Wong KC (1957). "Isolation of trachoma virus in chick embryo". J Hyg Epidemiol Microbiol Immunol. 1 (2): 109–20. PMID 13502539. - 1 2 Fredlund H, Falk L, Jurstrand M, Unemo M (2004). "Molecular genetic methods for diagnosis and characterisation of Chlamydia trachomatis and Neisseria gonorrhoeae: impact on epidemiological surveillance and interventions". APMIS: acta pathologica, microbiologica, et immunologica Scandinavica. 112 (11–12): 771–84. doi:10.1111/j.1600-0463.2004.apm11211-1205.x. PMID 15638837.
- ↑ Carlson JH, Whitmire WM, Crane DD, et al. (June 2008). "The Chlamydia trachomatis Plasmid Is a Transcriptional Regulator of Chromosomal Genes and a Virulence Factor". Infection and immunity. 76 (6): 2273–83. doi:10.1128/IAI.00102-08. PMC 2423098
 . PMID 18347045.
. PMID 18347045. - ↑ Harris SR, Clarke IN, Seth-Smith HM, et al. (April 2012). "Whole-genome analysis of diverse Chlamydia trachomatis strains identifies phylogenetic relationships masked by current clinical typing". Nat. Genet. 44 (4): 413–9, S1. doi:10.1038/ng.2214. PMC 3378690
 . PMID 22406642.
. PMID 22406642. - ↑ Ortiz L, Angevine M, Kim SK, Watkins D, DeMars R (2000). "T-Cell Epitopes in Variable Segments of Chlamydia trachomatis Major Outer Membrane Protein Elicit Serovar-Specific Immune Responses in Infected Humans". Infect. Immun. 68 (3): 1719–23. doi:10.1128/IAI.68.3.1719-1723.2000. PMC 97337
 . PMID 10678996.
. PMID 10678996. - 1 2 3 4 Malhotra M, Sood S, Mukherjee A, Muralidhar S, Bala M (September 2013). "Genital Chlamydia trachomatis: an update". Indian J. Med. Res. 138 (3): 303–16. PMC 3818592
 . PMID 24135174.
. PMID 24135174. - ↑ "Trachoma". Prevention of Blindness and Visual Impairment. World Health Organization.
- 1 2 "Chlamydia Trachomatis Infections: Screening, Diagnosis, and Management". American Family Physician. 86(12):1127-1132. 15 December 2012.
- ↑ Global Network for Neglected Tropical Diseases. Trachoma interactive fact sheet.http://old.globalnetwork.org/sites/all/modules/globalnetwork/factsheetxml/disease.php?id=9. Accessed February 6, 2011
- ↑ "Chlamydia Tests". Sexual Conditions Health Center. WebMD. Retrieved 2012-08-07.
Further reading
Bellaminutti, Serena; Seracini, Silva; De Seta, Francesco; Gheit, Tarik; Tommasino, Massimo; Comar, Manola (November 2014). "HPV and Chlamydia trachomatis Co-Detection in Young Asymptomatic Women from High Incidence Area for Cervical Cancer". Journal of Medical Virology. 86 (11): 1920–1925. doi:10.1002/jmv.24041. Retrieved 13 November 2014.
External links
- Chlamydiae.com
- 342556674 at GPnotebook
- "Chlamydia trachomatis". NCBI Taxonomy Browser. 813.
- Type strain of Chlamydia trachomatis at BacDive - the Bacterial Diversity Metadatabase