Breast cancer management
Breast cancer treatment takes different approaches depending on the conditions. The mainstay of breast cancer treatment is surgery when the tumor is localized, followed by chemotherapy (when indicated), radiotherapy, and, for ER-positive tumours, adjuvant hormonal therapy (with tamoxifen or an aromatase inhibitor). Management of breast cancer is undertaken by a multidisciplinary team based on national and international guidelines. Depending on clinical criteria (age, type of cancer, size, presence or absence of metastasis) patients are roughly divided to high risk and low risk cases, with each risk category following different rules for therapy. Treatment possibilities include radiation therapy, chemotherapy, hormone therapy, and immune therapy.
Staging
A patient generally first goes through a staging process to see if s/he can benefit from local treatment. Staging makes use of clinical, imaging and pathological assessment to make a best guess by the physician. If the cancer has spread beyond the breast and the lymph nodes then it is classified as Stage 4 or metastatic cancer and requires mostly systemic treatment.
Medical specialty professional organizations recommend against a physician's use of PET scans, CT scans, or bone scans when staging early breast cancer with low risk for metastasis.[1][2] The rationale is that there is no evidence which shows that extra testing results in better outcomes for a patient, but a patient who does receive tests against the consensus of professionals in the field is more likely to receive invasive procedures, overutilization of medical services, unnecessary radiation exposure, and experience misdiagnosis.[1][2]
Surgery
Depending on the staging and type of the tumor, just a lumpectomy (removal of the lump only) may be all that is necessary, or removal of larger amounts of breast tissue may be necessary. Surgical removal of the entire breast is called mastectomy.
Lumpectomy techniques are increasingly utilized for breast-conservation cancer surgery. Studies indicate that for patients with a single tumor smaller than 4 cm, lumpectomy may be as effective as a mastectomy.[3] Prior to a lumpectomy, a needle-localization of the lesion with placement of a guidewire may be performed, sometimes by a radiologist if the area being removed was detected by mammography or ultrasound, and sometimes by the surgeon if the lesion can be directly palpated.
However, mastectomy may be the preferred treatment in certain instances:
- Two or more tumors exist in different areas of the breast (a "multifocal" cancer).
- The breast has previously received radiotherapy.
- The tumor is large relative to the size of the breast.
- The patient has had scleroderma or another disease of the connective tissue, which can complicate radiotherapy.
- The patient lives in an area where radiotherapy is inaccessible.
- The patient is apprehensive about the risk of local recurrence after lumpectomy.
Standard practice requires the surgeon to establish that the tissue removed in the operation has margins clear of cancer, indicating that the cancer has been completely excised. If the removed tissue does not have clear margins, further operations to remove more tissue may be necessary. This may sometimes require removal of part of the pectoralis major muscle, which is the main muscle of the anterior chest wall.
During the operation, the lymph nodes in the axilla are also considered for removal. In the past, large axillary operations took out 10 to 40 nodes to establish whether cancer had spread. This had the unfortunate side effect of frequently causing lymphedema of the arm on the same side, as the removal of this many lymph nodes affected lymphatic drainage. More recently, the technique of sentinel lymph node (SLN) dissection has become popular, as it requires the removal of far fewer lymph nodes, resulting in fewer side effects. The sentinel lymph node is the first node that drains the tumor, and subsequent SLN mapping can save 65-70% of patients with breast cancer from having a complete lymph node dissection for what could turn out to be a negative nodal basin. Advances in Sentinel Lymph Node mapping over the past decade have increased the accuracy of detecting Sentinel Lymph Node from 80% using blue dye alone to between 92% and 98% using combined modalities.[4] SLN biopsy is indicated for patients with T1 and T2 lesions (<5 cm) and carries a number of recommendations for use on patient subgroups.[4] Recent trends continue to favor less radical axillar node resection even in the presence of some metastases in the sentinel node.[5]
Live tissue samples for testing
Recently live tissue samples from surgery are tested with various chemotherapy agents to derive probabilities of which ones may work better and especially the ones which would not work (cell-death assays). The companies need the sample within 24 hours of surgical excision. This is especially useful for early stage cancers where a response for the therapy cannot be determined once the whole cancer is taken out during the surgery and the chemotherapy is given in an adjuciant setting. However, the benefits of such tests have not yet been established in clinical trials and is not mainstream.
Lymphedema
Some patients develop lymphedema, as a result of axillary node dissection or of radiation treatment to the lymph nodes.[6] Although traditional recommendations limited exercise, a new study shows that participating in a safe, structured weight-lifting routine can help women with lymphedema take control of their symptoms and reap the many rewards that resistance training has on their overall health as they begin life as a cancer survivor. It recommends that women start with a slowly progressive program, supervised by a certified fitness professional, in order to learn how to do these types of exercises properly. Women with lymphedema should also wear a well-fitting compression garment during all exercise sessions.[7]
Radiation therapy
Radiation therapy is an adjuvant treatment for most women who have undergone lumpectomy and for some women who have mastectomy surgery. In these cases the purpose of radiation is to reduce the chance that the cancer will recur. Radiation therapy involves using high-energy X-rays or gamma rays that target a tumor or post surgery tumor site. This radiation is very effective in killing cancer cells that may remain after surgery or recur where the tumor was removed.
Radiation therapy can be delivered by either external beam radiotherapy or brachytherapy (internal radiotherapy). In the case of external beam radiotherapy, X-rays are delivered from outside the body by a machine called a Linear Accelerator or Linac. In contrast, brachytherapy involves the precise placement of radiation source(s) directly at the treatment site. Radiation therapy for breast cancer is usually performed after surgery and is an integral component of breast-conserving therapy.
Radiation therapy eliminates the microscopic cancer cells that may remain near the area where the tumor was surgically removed. The dose of radiation must be strong enough to ensure the elimination of cancer cells. However, radiation affects normal cells and cancer cells alike, causing some damage to the normal tissue around where the tumor was. Healthy tissue can repair itself, while cancer cells do not repair themselves as well as normal cells. For this reason, radiation treatments are given over an extended period, enabling the healthy tissue to heal. Treatments using external beam radiotherapy are typically given over a period of five to seven weeks, performed five days a week. Recent large trials (UK START and Canadian) have confirmed that shorter treatment courses, typically over three to four weeks, result in equivalent cancer control and side effects as the more protracted treatment schedules. Each treatment takes about 15 minutes. A newer approach, called 'accelerated partial breast irradiation' (APBI), uses brachytherapy to deliver the radiation in a much shorter period of time. APBI delivers radiation to only the immediate region surrounding the original tumor[8][9][10] and can typically be completed over the course of one week.[8]
Indications for radiation
Radiation treatment is mainly effective in reducing the risk of local relapse in the affected breast. Therefore, it is recommended in most cases of breast conserving surgeries and less frequently after mastectomy. Indications for radiation treatment are constantly evolving. Patients treated in Europe have been more likely in the past to be recommended adjuvant radiation after breast cancer surgery as compared to patients in North America. Radiation therapy is usually recommended for all patients who had lumpectomy, quadrant-resection. Radiation therapy is usually not indicated in patients with advanced (stage IV disease) except for palliation of symptoms like bone pain or fungating lesions.
In general recommendations would include radiation:
- As part of breast conserving therapy.
- After mastectomy for patients with higher risk of recurrence because of conditions such as a large primary tumor or substantial involvement of the lymph nodes.[11]
Other factors which may influence adding adjuvant radiation therapy:
- Tumor close to or involving the margins on pathology specimen
- Multiple areas of tumor (multicentric disease)
- Microscopic invasion of lymphatic or vascular tissues
- Microcopic invasion of the skin, nipple/areola, or underlying pectoralis major muscle
- Patients with extension out of the substance of a LN
- Inadequate numbers of axillary LN sampled
Types of radiotherapy

Radiotherapy can be delivered in many ways but is most commonly produced by a linear accelerator.
This usually involves treating the whole breast in the case of breast lumpectomy or the whole chest wall in the case of mastectomy. Lumpectomy patients with early-stage breast cancer may be eligible for a newer, shorter form of treatment called "breast brachytherapy". This approach allows physicians to treat only part of the breast in order to spare healthy tissue from unnecessary radiation.
Improvements in computers and treatment delivery technology have led to more complex radiotherapy treatment options. One such new technology is using IMRT (intensity modulated radiation therapy), which can change the shape and intensity of the radiation beam making "beamlets" at different points across and inside the breast. This allows for better dose distribution within the breast while minimizing dose to healthy organs such as the lung or heart.[12] However, there is yet to be a demonstrated difference in treatment outcomes (both tumor recurrence and level of side effects) for IMRT in breast cancer when compared to conventional radiotherapy treatment. In addition, conventional radiotherapy can also deliver similar dose distributions utilizing modern computer dosimetry planning and equipment. External beam radiation therapy treatments for breast cancer are typically given every day, five days a week, for five to 10 weeks.[13]
Within the past decade, a new approach called accelerated partial breast irradiation (APBI) has gained popularity. APBI is used to deliver radiation as part of breast conservation therapy. It treats only the area where the tumor was surgically removed, plus adjacent tissue. APBI reduces the length of treatment to just five days, compared to the typical six or seven weeks for whole breast irradiation.
APBI treatments can be given as brachytherapy or external beam with a linear accelerator. These treatments are usually limited to women with well-defined tumors that have not spread.[14] A meta-analysis of randomised trials of partial breast irradiation (PBI) vs. whole breast irradiation (WBI) as part of breast conserving therapy demonstrated a reduction in non-breast-cancer and overall mortality.[15] Full text and Audio Slides
In breast brachytherapy, the radiation source is placed inside the breast, treating the cavity from the inside out. There are several different devices that deliver breast brachytherapy. Some use a single catheter and balloon to deliver the radiation. Other devices utilize multiple catheters to deliver radiation.
A study is currently underway by the National Surgical Breast and Bowel Project (NSABP) to determine whether limiting radiation therapy to only the tumor site following lumpectomy is as effective as radiating the whole breast.
New technology has also allowed more precise delivery of radiotherapy in a portable fashion — for example in the operating theatre. Targeted intraoperative radiotherapy (TARGIT)[16] is a method of delivering therapeutic radiation from within the breast using a portable X-ray generator called Intrabeam.
The TARGIT-A trial was an international randomised controlled non-inferiority phase III clinical trial led from University College London. 28 centres in 9 countries accrued 2,232 patients to test whether TARGIT can replace the whole course of radiotherapy in selected patients.[17] The TARGIT-A trial results found that the difference between the two treatments was 0.25% (95% CI -1.0 to 1.5) i.e., at most 1.5% worse or at best 1.0% better with single dose TARGIT than with standard course of several weeks of external beam radiotherapy.[18] In the TARGIT-B trial, as the TARGIT technique is precisely aimed and given immediately after surgery, in theory it could be able provide a better boost dose to the tumor bed as suggested in phase II studies.[19]
Side effects of radiation therapy
External beam radiation therapy is a non-invasive treatment with some short term and some longer-term side effects. Patients undergoing some weeks of treatment usually experience fatigue caused by the healthy tissue repairing itself and aside from this there can be no side effects at all. However many breast cancer patients develop a suntan-like change in skin color in the exact area being treated. As with a suntan, this darkening of the skin usually returns to normal in the one to two months after treatment. In some cases permanent changes in color and texture of the skin is experienced. Other side effects sometimes experienced with radiation can include:
- muscle stiffness
- mild swelling
- tenderness in the area
- lymphedema
After surgery, radiation and other treatments have been completed, many patients notice the affected breast seems smaller or seems to have shrunk. This is basically due to the removal of tissue during the lumpectomy operation.
The use of adjuvant radiation has significant potential effects if the patient has to later undergo breast reconstruction surgery. Fibrosis of chest wall skin from radiation negatively affects skin elasticity and makes tissue expansion techniques difficult. Traditionally most patients are advised to defer immediate breast reconstruction when adjuvant radiation is planned and are most often recommended surgery involving autologous tissue reconstruction rather than breast implants.
Studies suggest APBI may reduce the side effects associated with radiation therapy, because it treats only the tumor cavity and the surrounding tissue. In particular, a device that uses multiple catheters and allows modulation of the radiation dose delivered by each of these catheters has been shown to reduce harm to nearby, healthy tissue.[20]
Systemic therapy
Systemic therapy uses medications to treat cancer cells throughout the body. Any combination of systemic treatments may be used to treat breast cancer. Systemic treatments include chemotherapy, immune therapy, and hormonal therapy.
Chemotherapy
Chemotherapy (drug treatment for cancer) may be used before surgery, after surgery, or instead of surgery for those cases in which surgery is considered unsuitable.
Hormonal Receptor Status
Women who have had breast cancer are at increased risk of a second primary breast cancer, compared with risk in the general population.
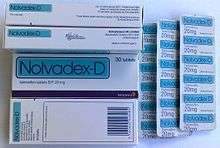
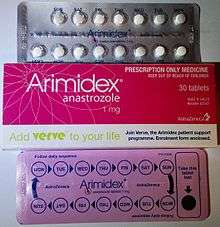
Patients with estrogen receptor positive tumors will typically receive hormonal therapy after chemotherapy is completed. Typical hormonal treatments include:
- Tamoxifen is typically given to premenopausal women to inhibit the estrogen receptors.
- Aromatase inhibitors are typically given to postmenopausal women to lower the amount of estrogen in their systems.
- GnRH-analogues for ovarian suppression are beneficial in women who remain premenopausal and are at sufficient risk for recurrence to warrant adjuvant chemotherapy.[21]
- Estrogen cycling was reported at the 31st annual San Antonio Breast Cancer Symposium. About a third of the 66 participants - women with metastatic breast cancer that had developed resistance to standard estrogen-lowering therapy - a daily dose of estrogen could stop the growth of their tumors or even cause them to shrink. If study participants experienced disease progression on estrogen, they could go back to an aromatase inhibitor that they were previously resistant to and see a benefit - their tumors were once again inhibited by estrogen deprivation. That effect sometimes wore off after several months, but then the tumors might again be sensitive to estrogen therapy. In fact, some patients have cycled back and forth between estrogen and an aromatase inhibitor for several years. PET (positron emission tomography) scans before starting estrogen and again 24 hours later predicted those tumors which responded to estrogen therapy: the responsive tumors showed an increased glucose uptake, called a PET flare. The mechanism of action is uncertain, although estrogen reduces the amount of a tumor-promoting hormone called insulin-like growth factor-1 (IGF1).[22]
Targeted therapy
In patients whose cancer expresses an over-abundance of the HER2 protein, a monoclonal antibody known as trastuzumab (Herceptin) is used to block the activity of the HER2 protein in breast cancer cells, slowing their growth. In the advanced cancer setting, trastuzumab use in combination with chemotherapy can both delay cancer growth as well as improve the recipient's survival.[23]
Antiangiogenic therapy
A commercially available monoclonal antibody that blocks the activation of the VEGF receptor, bevacizumab, underwent testing in a randomized clinical trial whose preliminary results were announced by the National Cancer Institute in 2005.[24] The preliminary data indicated that bevacizumab delays disease progression for up to five months over conventional chemotherapy, but survival was no better. Genentech, manufacturer of bevacizumab, has filed a supplemental biological application with the US FDA for approval of bevacizumab in the setting of metastatic breast cancer, on the strength of the improvement in progression-free survival.
Immunotherapy
The cancer immunotherapy can help the immune system fight tumors.[25]
Dendritic cell therapy
A new clinical trial is designed around the use of QI's proprietary dendritic cell therapy, which employs oncofetal antigen ("OFA") to recruit the patient's own immune system to target and attack the cancer cells with the intent to improve patient survivability and quality of life. Each patient will receive three monthly injections of the patient's own dendritic cells that have been sensitized to OFA. It is anticipated that once the sensitized cells are injected back into the patient, the patient's T-cells will locate the OFA found on the patient's cancer cells, thereby generating an immune response with the goal of killing the cancer cells and preventing further spread of the disease.[26]
Stimuvax - mostly for hormone receptor positive (phase III)
Stimuvax is an investigational therapeutic cancer vaccine designed to induce an immune response to cancer cells that express MUC1, a glycoprotein antigen widely expressed on common cancers. MUC1 is over-expressed on many cancers such as lung cancer, breast cancer, prostate cancer and colorectal cancer. Stimuvax is thought to work by stimulating the body's immune system to identify and destroy cancer cells expressing MUC1.[27]
Phase IIb study of 171 patients with inoperable stage IIIb NSCLC (lung cancer), in which Stimuvax showed a trend towards extending median overall survival from 13.3 months for patients receiving best supportive care (BSC) to 30.6 months for patients receiving Stimuvax plus BSC.2,3 Reported side effects included mild-to-moderate flu-like symptoms, gastrointestinal disturbances and mild injection-site reactions.
Chemoimmunotherapy
Manipulating the immune system to recognize and eradicate breast tumor cells is a highly attractive alternative approach to disease management. Active immunization offers multiple theoretical advantages over all other therapies, including low toxicity. The sustained antitumor effect due to immunological memory would obviate the requirement for prolonged, repetitive cycles of therapy.
The objective of chemoimmunotherapy is to amplify natural pre-existing T cell responses specific for any known or unknown tumor antigen and to recruit and amplify new tumor-specific T cell responses resulting from the use of cytotoxic drugs. The direct cytolytic effect of some cytotoxic drugs, such as paclitaxel, can enhance antigen presentation by inducing tumor cell apoptosis. This mechanism of therapeutic synergy has been shown with cyclophosphamide, doxorubicin, or paclitaxel when given with dendritic cell - based vaccines. Until 9 years ago, it was thought that the T cell depletion caused by chemotherapy would make immunotherapy ineffective. However it has now been shown that, on the contrary, the vigorous T cell repopulation following depletion can be directed against the tumor.
IMP321 induced both a sustained increase in the number and activation of APC (monocytes and dendritic cells) and an increase in the percentage of NK and long-lived cytotoxic effector-memory CD8 T cells. Clinical benefit was observed for 90 per cent of patients with only 3 progressors at 6 months. Also, the objective tumor response rate of 50 per cent compared favorably to the 25 per cent rate reported in the historical control group. This form of chemo-immunotherapy should be applicable to many chemotherapies.[28]
Thermochemotherapy
Medifocus heat treatment added to Standard of Care (SoC) chemotherapy increased the median tumor shrinkage in the thermochemotherapy arm to 88.4%, while for chemotherapy alone the median tumor shrinkage was 58.8%. For the thermo-chemotherapy treatment arm, almost 80% of breast tumors had a tumor volume reduction of 80% or more, compared to only 20% for the chemotherapy alone.[29]
Alternative treatments
Doctors have begun treating women suffering from breast cancer with a procedure known as cryoablation. The treatment freezes, than defrosts tumors using small needles so that only the harmful tissue is damaged and ultimately dies.[30] The advantage of this technique includes alternative to surgery, limiting hospital visits and reducing scarring.
Gene expression profiling
Gene expression profiling of breast tumors can predict the chances of developing breast cancer again. The most useful setting for these tests is where the benefit of chemotherapy is felt to be small. In up to 10% of patients, there will be disease recurrences, but treating every patient with chemotherapy is overkill. In this setting, a high-risk score can help doctors decide whether to recommend chemotherapy.
Treatment response assessment
Physical examination and conventional imaging techniques still have an important place in the evaluation of breast cancer treated by neoadjuvant chemotherapy. At this time, this morphologic evaluation is the only one recognized by the international criteria. The new functional and metabolic imaging modalities, particularly MRI and PET scan, can approach the nature of residual tumour, allow early detection of bad responders and depict multifocal tumours and metastases.[31]
- Using PET/CT Imaging, UCLA Cancer Researchers Can Tell After A Single Cycle Of Chemotherapy Whether Drugs Are Working[32]
- MRI accurately detects residual breast tumors after radiofrequency ablation[33]
- water diffusion MRI — a potential new biomarker of response to cancer therapy[34]
- CK18 biomarkers are useful for early prediction of the response to CEF therapy in breast cancer and may be useful biomarkers for clinical trials[35]
- 3T MRI depicted a significantly higher number of malignant tumors of the breast than mammography and sonography[36]
Blood test
The current standard of care for metastatic disease involves the use of radiology studies such as CT scans, ultrasounds, and the like to determine whether or not patients are deriving benefit from their current therapies. An alternative is the FDA-approved CellSearch technology, looking at circulating tumor cells (CTCs) in blood collected from women in need of a new treatment regimen for metastatic breast cancer. About one tablespoon of blood was collected when the patient started the new therapy, and then again at three to four-week intervals. The number of CTCs was correlated with disease response or progression as determined by standard radiology studies (e.g., CT scans) performed every nine to 12 weeks.[37]
Managing side effects
Drugs and radiotherapy given for cancer can cause unpleasant side effects such as nausea and vomiting, mouth sores, dermatitis, and menopausal symptoms. Around a third of patients with cancer use complementary therapies, including homeopathic medicines, to try to reduce these side effects.[38]
Insomnia
It was believed that one would find a bi-directional relationship between insomnia and pain, but instead it was found that trouble sleeping was more likely a cause, rather than a consequence, of pain in patients with cancer. An early intervention to manage sleep would overall relieve patient with side effects.[39]
Approximately 40 percent of menopausal women experience sleep disruption, often in the form of difficulty with sleep initiation and frequent nighttime awakenings. There is a study, first to show sustained benefits in sleep quality from gabapentin, which Rochester researchers already have demonstrated alleviates hot flashes.[40]
Hot flushes
Lifestyle adjustments are usually suggested first to manage hot flushes (or flashes) due to endocrine therapy.[41] This can include avoiding triggers such as alcohol, caffeine and smoking. If hot flashes continue, and depending on their frequency and severity, several drugs can be effective in some patients, in particular SNRIs such as venlafaxine, also oxybutinin and others.
Complementary medicines that contain phytoestrogens are not recommended for breast cancer patients as they may stimulate oestrogen receptor-positive tumours.[42]
Lymphedema
The lymphatic system is a transport system similar to the circulatory system but with the difference that it transports lymph instead of blood. The lymph is a fluid rich mainly in white blood cells and proteins with a specific task to collect viruses, bacteria, and waste products in order to flush them from our body. When our lymphatic system is damaged or blocked, a chronic and progressive stage of swelling is activated within the soft tissue. This swelling is known as “lymphedema” and it can be classified in two, primary and secondary. Primary lymphedema is a non-common type of lymphedema since it is an inherited condition. On the other hand, the secondary lymphedema is a condition in which the lymph nodes have been affected and damaged due to many conditions, e.g. surgery, radiation, infection, cancer. There are over 11 million cancer survivors in the U.S. that have been submitted to radiation, surgery, and/or chemotherapy. Interestingly, it has been shown in the literature that lymphedema may occur within days and up to 30 years after treatment for breast cancer. Also, 80% of patients experience onset within 3 years of surgery. Lymphedema can affect both, upper and lower extremities. Upper-extremity lymphedema most often occurs after breast cancer; lower-extremity lymphedema most often occurs with uterine cancer, prostate cancer, lymphoma, or melanoma. In physical therapy, specialized lymphedema therapists manage this condition through decongestive therapy. This is a method based on manual lymphatic drainage, compression, skin care, and decongestive exercise. The right order and progression of treatment is stipulated by the lymphedema therapist, who will precede the lymphedema management mainly by its stage. One of the biggest myths from the past is that a person at risk for lymphedema or who has it should not carry heavy objects. Moreover, a person undergoing lymphedema should not exercise while wearing a compression garment. It is very important to point out that exercise training is a physiological stress to the body. The main purpose of exercise is to increase the capacity of the exercised body system to respond to future stresses. Decongestive exercise will be prescribed by the lymphedema therapist during the management of the condition. The exercises should be performed wearing compression bandages or compression sleeves/garments. There is a gap in the literature explaining and showing more in depth the positive results of exercise and compression in lymphedema patients. Some papers say that “the combination of exercise with compression garments is considered to add an effect on lymph flow from the affected limb acting as a counterforce to the muscle contractions, which are the most important stimulus to lymph flow” but they also mentioned that “the compression sleeve may also limit capillary filtration by opposing capillary pressure.” So going back to our main question, does exercise training increase the risk of lymphedema in cancer survivors? The answer is NO. The purpose of the compression for lymphedema management is mainly to improve the lymphatic and venous return and prevent reaccumulation of the evacuated. It basically serves as constant compression gradient to maintain the reduction of the edema and encourage the flow of lymphatic fluid out of the limb(s). When a person performs exercise while wearing any kind of compression system according to the stage of lymphedema, the compression properties plus the effect of muscle and joint pumping will help to return fluids within the venous and lymphatic system. These facts let us assure that exercise training does not produce more lymphedema or increases the risk of lymphedema in cancer survivors. Patients have to be aware of the benefits but more importantly, they have to be treated by a certified lymphedema therapist in order to achieve the right goals.
Beesley, V., Janda, M., Eakin, E., Obermair, A., & Battistutta, D. (2007). Lymphedema after gynecological cancer treatment. Cancer, 109(12), 2607-2614. Brennan, M. J., & Miller, L. T. (1998). Overview of treatment options and review of the current role and use of compression garments, intermittent pumps, and exercise in the management of lymphedema. Cancer, 83(S12B), 2821-2827. Courneya, K. S., Segal, R. J., Mackey, J. R., Gelmon, K., Reid, R. D., Friedenreich, C. M., . . . Lane, K. (2007). Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. Journal of Clinical Oncology, 25(28), 4396-4404. Harris, S. R., & Niesen‐Vertommen, S. L. (2000). Challenging the myth of exercise‐induced lymphedema following breast cancer: A series of case reports. Journal of Surgical Oncology, 74(2), 95-98. Johansson, K., Tibe, K., Weibull, A., & Newton, R. (2005). Low intensity resistance exercise for breast cancer patients with arm lymphedema with or without compression sleeve. Lymphology, 38(4), 167-180. Meneses, K. D., & McNees, M. P. (2007). Upper extremity lymphedema after treatment for breast cancer: a review of the literature. Ostomy/wound management, 53(5), 16-29. Petrek, J. A., Senie, R. T., Peters, M., & Rosen, P. P. (2001). Lymphedema in a cohort of breast carcinoma survivors 20 years after diagnosis. Cancer, 92(6), 1368-1377. Schmitz, K. H. (2010). Balancing lymphedema risk: exercise versus deconditioning for breast cancer survivors. Exercise and sport sciences reviews, 38(1), 17. Shaw, C., Mortimer, P., & Judd, P. A. (2007). Randomized controlled trial comparing a low‐fat diet with a weight‐reduction diet in breast cancer‐related lymphedema. Cancer, 109(10), 1949-1956. Zuther, J. (2005). Comprehensive Lymphedema Management. Thieme Medical Publishers.
Reoccurrence monitoring
Chronix Biomedical has reported new data further demonstrating that its serum DNA blood tests have the potential to accurately detect early stage breast cancer and prostate cancer. Chronix's proprietary technology identifies disease-specific genetic fingerprints based on circulating DNA fragments that are released into the bloodstream by damaged and dying (apoptotic) cells.
The tests use proprietary algorithms developed by Chronix researchers to detect, analyze and identify cancer-related fragments of circulating DNA that are released into the bloodstream by apoptotic cells. Chronix researchers consistently find that this apoptotic DNA in the serum is coming from a limited number of regions or "hotspots" on the genome specific to each cancer. According to the data presented today, DNA fragments from any one of the 29 breast cancer "hotspots" and 32 prostate cancer "hotspots" identified by Chronix researchers indicate that cancer is present.[43]
See also
- ALMANAC, Axillary Lymphatic Mapping Against Nodal Axillary Clearance trial
References
- 1 2 American Society of Clinical Oncology, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Society of Clinical Oncology, retrieved 14 August 2012
- 1 2 Carlson, R. W.; Allred, D. C.; Anderson, B. O.; Burstein, H. J.; Carter, W. B.; Edge, S. B.; Erban, J. K.; Farrar, W. B.; Goldstein, L. J.; Gradishar, W. J.; Hayes, D. F.; Hudis, C. A.; Jahanzeb, M.; Kiel, K.; Ljung, B. M.; Marcom, P. K.; Mayer, I. A.; McCormick, B.; Nabell, L. M.; Pierce, L. J.; Reed, E. C.; Smith, M. L.; Somlo, G.; Theriault, R. L.; Topham, N. S.; Ward, J. H.; Winer, E. P.; Wolff, A. C.; NCCN Breast Cancer Clinical Practice Guidelines Panel (2009). "Breast cancer. Clinical practice guidelines in oncology". Journal of the National Comprehensive Cancer Network : JNCCN. 7 (2): 122–192. PMID 19200416.
- ↑ "Mastectomy vs. Lumpectomy". Breastcancer.org. 9 June 2013. Retrieved 23 October 2013.
- 1 2 Bennett, Joseph J. (2006). "Sentinel Lymph Node Biopsy for Breast Cancer and Melanoma". US Oncological Disease. 1 (1): 16–19. Retrieved 23 October 2013.
- ↑ Giuliano, A. E.; Hunt, K. K.; Ballman, K. V.; Beitsch, P. D.; Whitworth, P. W.; Blumencranz, P. W.; Leitch, A. M.; Saha, S.; McCall, L. M.; Morrow, M. (2011). "Axillary Dissection vs No Axillary Dissection in Women with Invasive Breast Cancer and Sentinel Node Metastasis: A Randomized Clinical Trial". JAMA: the Journal of the American Medical Association. 305 (6): 569–575. doi:10.1001/jama.2011.90. PMID 21304082.
- ↑ "Causes, incidence, and risk factors". Lymphatic obstruction. U.S. National Library of Medicine. 3 September 2012. Retrieved 23 October 2013.
- ↑ "Lifting Weights Reduces Lymphedema Symptoms Following Breast Cancer Surgery". Medical News Today. 13 August 2009. Retrieved 23 October 2013.
- 1 2 Nelson, J. C.; Beitsch, P. D.; Vicini, F. A.; Quiet, C. A.; Garcia, D.; Snider, H. C.; Gittleman, M. A.; Zannis, V. J.; Whitworth, P. W.; Fine, R. E.; Keleher, A. J.; Kuerer, H. M. (2009). "Four-year clinical update from the American Society of Breast Surgeons MammoSite brachytherapy trial". The American Journal of Surgery. 198 (1): 83–91. doi:10.1016/j.amjsurg.2008.09.016. PMID 19268900.
- ↑ Keisch; et al. (February 2007). "American Brachytherapy Society breast brachytherapy task group" (PDF). American Brachytherapy Society. Retrieved 25 September 2009.
- ↑ Polgár, C.; Major, T. (2009). "Current status and perspectives of brachytherapy for breast cancer". International Journal of Clinical Oncology. 14 (1): 7–0. doi:10.1007/s10147-008-0867-y. PMID 19225919.
- ↑ "Radiation After Mastectomy". RT Answers. Retrieved 23 October 2013.
- ↑ "External Beam Radiation Therapy". RT Answers. Retrieved 23 October 2013.
- ↑ "External Beam Radiation Therapy after Lumpectomy". RT Answers. Retrieved 23 October 2013.
- ↑ "Accelerated Partial Breast Irradiation". RT Answers. Retrieved 23 October 2013.
- ↑ Vaidya, Jayant S.; Bulsara, Max; Wenz, Frederik; Coombs, Nathan; Singer, Julian; Ebbs, Stephen; Massarut, Samuele; Saunders, Christobel; Douek, Michael; Williams, Norman; Joseph, David; Tobias, Jeffrey S.; Baum, Michael (May 2016). "Reduced mortality with partial breast irradiation for early breast cancer – a meta-analysis of randomised trials". International Journal of Radiation Oncology*Biology*Physics. doi:10.1016/j.ijrobp.2016.05.008.
- ↑ Vaidya J. "TARGIT (TARGeted Intraoperative radioTherapy)". Retrieved 2007-03-11.
- ↑ Vaidya J, Tobias J, Baum M, Houghton J. "Protocol 99PRT/47 Targeted Intraoperative radiotherapy (Targit) for breast cancer". Retrieved 2007-03-11.
- ↑ Vaidya, Jayant S; Joseph, David J; Tobias, Jeffrey S; Bulsara, Max; Wenz, Frederik; Saunders, Christobel; Alvarado, Michael; Flyger, Henrik L; Massarut, Samuele; Eiermann, Wolfgang; Keshtgar, Mohammed; Dewar, John; Kraus-Tiefenbacher, Uta; Sütterlin, Marc; Esserman, Laura; Holtveg, Helle MR; Roncadin, Mario; Pigorsch, Steffi; Metaxas, Marinos; Falzon, Mary; Matthews, April; Corica, Tammy; Williams, Norman R; Baum, Michael (1 July 2010). "Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial". The Lancet. 376 (9735): 91–102. doi:10.1016/S0140-6736(10)60837-9. PMID 20570343.
- ↑ Vaidya, J. S.; Baum, M.; Tobias, J. S.; Massarut, S.; Wenz, F.; Murphy, O.; Hilaris, B.; Houghton, J.; Saunders, C.; Corica, T.; Roncadin, M.; Kraus-Tiefenbacher, U.; Melchaert, F.; Keshtgar, M.; Sainsbury, R.; Douek, M.; Harrison, E.; Thompson, A.; Joseph, D. (2006). "Targeted intraoperative radiotherapy (TARGIT) yields very low recurrence rates when given as a boost". International Journal of Radiation Oncology*Biology*Physics. 66 (5): 1335–1338. doi:10.1016/j.ijrobp.2006.07.1378. PMID 17084562.
- ↑ Yashar, Catheryn M.; Blair, Sarah; Wallace, Anne; Scanderbeg, Dan (1 October 2009). "Initial clinical experience with the Strut-Adjusted Volume Implant brachytherapy applicator for accelerated partial breast irradiation". Brachytherapy. 8 (4): 367–372. doi:10.1016/j.brachy.2009.03.190. PMID 19744892.
- ↑ Francis, Prudence A.; Regan, Meredith M.; Fleming, Gini F.; Láng, István; Ciruelos, Eva; Bellet, Meritxell; Bonnefoi, Hervé R.; Climent, Miguel A.; Prada, Gian Antonio Da; Burstein, Harold J.; Martino, Silvana; Davidson, Nancy E.; Geyer, Charles E.; Walley, Barbara A.; Coleman, Robert; Kerbrat, Pierre; Buchholz, Stefan; Ingle, James N.; Winer, Eric P.; Rabaglio-Poretti, Manuela; Maibach, Rudolf; Ruepp, Barbara; Giobbie-Hurder, Anita; Price, Karen N.; Colleoni, Marco; Viale, Giuseppe; Coates, Alan S.; Goldhirsch, Aron; Gelber, Richard D. (2014). "Adjuvant Ovarian Suppression in Premenopausal Breast Cancer". New England Journal of Medicine: 141211053020000. doi:10.1056/NEJMoa1412379. ISSN 0028-4793.
- ↑ "Women With Metastatic Breast Cancer Can Benefit From Estrogen Pills". Medical News Today. 12 December 2008. Retrieved 23 October 2013.
- ↑ Slamon, D. J.; Leyland-Jones, B.; Shak, S.; Fuchs, H.; Paton, V.; Bajamonde, A.; Fleming, T.; Eiermann, W.; Wolter, J.; Pegram, M.; Baselga, J.; Norton, L. (2001). "Use of Chemotherapy plus a Monoclonal Antibody against HER2 for Metastatic Breast Cancer That Overexpresses HER2". New England Journal of Medicine. 344 (11): 783–792. doi:10.1056/NEJM200103153441101. PMID 11248153.
- ↑ "Bevacizumab Combined With Chemotherapy Improves Progression-Free Survival for Patients With Advanced Breast Cancer" (Press release). National Cancer Institute. 14 April 2005. Retrieved 2013-12-07.
- ↑ Hobohm, Uwe (1 January 2009). "Healing Heat: Harnessing Infection to Fight Cancer". American Scientist. 97 (1): 34. doi:10.1511/2009.76.34.
- ↑ "Quantum Immunologics Achieves Major Funding In Support Of Ongoing FDA Trials". Medical News Today. 17 July 2009. Retrieved 23 October 2013.
- ↑ "Oncothyreon Announces Initiation Of Phase 3 Trial Of Stimuvax In Breast Cancer". Medical News Today. 23 June 2009. Retrieved 23 October 2013.
- ↑ "Immutep Announces Final Results In Phase I/II Chemoimmunotherapy Trial In Metastatic Breast Cancer". Medical News Today. 7 September 2010. Retrieved 24 October 2013.
- ↑ "Medifocus, Inc. Announces Institutional Review Board (IRB) Approval For Its Phase III Pivotal Breast Cancer Treatment Study". Medical News Today. 22 October 2010. Retrieved 24 October 2013.
- ↑ Gray, Richard (9 December 2012). "Breast cancer could be treated by turning tumours into ball of ice". The Telegraph. Retrieved 24 October 2013.
- ↑ Ollivier, L.; Balu-Maestro, C.; Leclère, J. (2005). "Imaging in evaluation of response to neoadjuvant breast cancer treatment". Cancer Imaging. 5 (1): 27–31. doi:10.1102/1470-7330.2005.0009. PMC 1665221
 . PMID 16154816.
. PMID 16154816. - ↑ "Using PET/CT Imaging, UCLA Cancer Researchers Can Tell After A Single Cycle Of Chemotherapy Whether Drugs Are Working". Medical News Today. 16 April 2009. Retrieved 24 October 2013.
- ↑ Kerr, Martha (December 2, 2008). "MRI accurately detects residual breast tumors after radiofrequency ablation". AuntMinnie.com. Reuters Health.
- ↑ Koh, Dow-Mu; Collins, David J. (1 June 2007). "Diffusion-Weighted MRI in the Body: Applications and Challenges in Oncology". American Journal of Roentgenology. 188 (6): 1622–1635. doi:10.2214/AJR.06.1403.
- ↑ Olofsson, M. H.; Ueno, T.; Pan, Y.; Xu, R.; Cai, F.; van der Kuip, H.; Muerdter, T. E.; Sonnenberg, M.; Aulitzky, W. E.; Schwarz, S.; Andersson, E.; Shoshan, M. C.; Havelka, A. M.; Toi, M.; Linder, S. (1 June 2007). "Cytokeratin-18 Is a Useful Serum Biomarker for Early Determination of Response of Breast Carcinomas to Chemotherapy". Clinical Cancer Research. 13 (11): 3198–3206. doi:10.1158/1078-0432.CCR-07-0009. PMID 17545523.
- ↑ "3T MRI Detects "Early" Breast Cancer Not Seen On Mammography And Sonography". Medical News Today. 16 April 2009. Retrieved 24 October 2013.
- ↑ "Blood Test Helps Guide Treatment And Can Impact Quality Of Life For Breast Cancer Patients". Medical News Today. 17 September 2009. Retrieved 24 October 2013.
- ↑ "Can Homeopathic Medicines Help Relieve The Side-Effects Of Cancer Therapy?". Medical News Today. 15 April 2009. Retrieved 24 October 2013.
- ↑ "Treating Sleep Problems May Improve Pain Management In Patients With Cancer". Medical News Today. 16 April 2009. Retrieved 24 October 2013.
- ↑ "Sleep For Women With Hot Flashes Enhanced By Seizure Drug". Medical News Today. 9 September 2009. Retrieved 24 October 2013.
- ↑ See for example a review by Kligman and Younus "Management of hot flashes in women with breast cancer. Curr Oncol. Feb 2010; 17(1): 81–86.".
- ↑ For example National Prescribing Service NPS MedicineWise "Phytoestrogens for menopausal hot flushes.". | Published in Health News and Evidence 14 July 2014 | retrieved 25 August 2014
- ↑ "Chronix's Serum DNA Assays May Represent A New Approach To Diagnostics And Prognostics In Cancer And Other Diseases". Medical News Today. 8 June 2010. Retrieved 24 October 2013.
External links
- Breast cancer at DMOZ
- Prevention and treatment of breast cancer by suppressing aromatase activity and expression